I Have to Drive 6 Hours for Pain Care
/By Bailey Parker, Guest Columnist
I feel so alone and isolated. There have been times I wanted to die, but my 5-year old son keeps me going. I get up every day for him.
About two years after he was born, I had a car wreck. I hit a coyote at 60 mph and ripped the radiator off my car. The doctors told me I had the spine of an 80-year old and needed a double level fusion in my neck.
I was 34 then and in tremendous amounts of pain. But after reading online stories in spine health forums, I was skeptical about the surgery. Everything told me to wait. So I did, for a year. I saw three surgeons and a neurologist. They all told me to have the surgery.
I live in a small city in southwest Colorado. When it comes to opioid pain medication, all the doctors here seem to have taken the stance, “We just don’t do that here.” The nearest city is Albuquerque, New Mexico, which means a 4-hour drive for me across state lines, or a 6-hour drive to Denver over mountain passes.
Before my surgery, one of the doctors of orthopedic medicine prescribed my pain medication. For two months, I was able to work again and was beginning to get back on my feet. I remember thinking at the time that I didn’t want to take medication for the rest of my life, but the fusion sounded worse.
The third month in I called for a refill of my medication. They told me no, but wouldn’t say why or give me a follow up exam with the doctor. He was too busy and couldn’t see me for a month. I waited one excruciating month and went to see him, asking what happened.
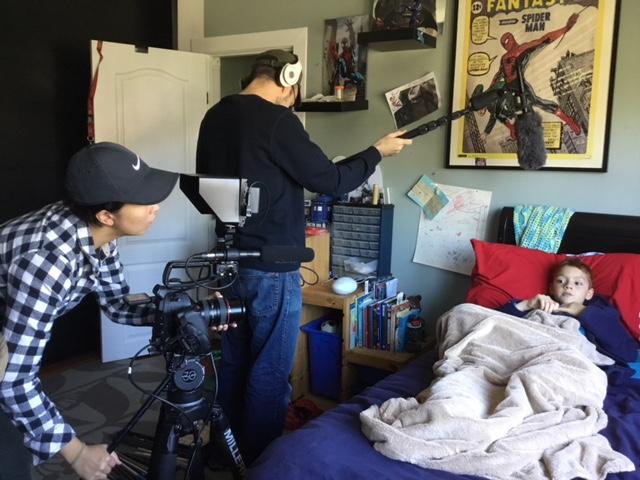
BAILEY PARKER
He had looked at my prescription records and saw a prescription for narcotics from another doctor for when I had cystic fibroids on my ovaries. It was not the same pain medication as what he prescribed me, and I didn’t even know they were the same type of medicine.
Even though I had a broken neck, he did not feel comfortable prescribing to me anymore. His office then took 6 months to get my medical records sent to my primary care doctor. I had to physically go in and yell at them that I was about to have major surgery. This was the first time I felt treated like an addict, but not the last.
I went to my primary care physician and explained what happened with this other doctor. We have a very good relationship. She knows all of my medical history. She handled my pain medication before my surgery but was very clear that she would not do it for an extended period.
I never take more medication than prescribed. I am not an addict. I do everything they tell me. I was walking and doing yoga every day, just as the doctors recommended. I took my vitamins and a fruit shake every day.
After the fusion surgery, things just didn’t feel right. I was in tremendous pain again and this time there was more of it in different places. I told the physician’s assistant at my surgeon’s office and he told me to just get off all the drugs. He said it would help. He told me I would be fine. I wasn’t.
I struggled for another month before I demanded to see the surgeon. He told me I would benefit from OxyContin and gave me a week’s supply. For the first time since my accident, I was able to work and properly care for my son. My depression lifted. But when I called to tell them that I was doing good on the medication, they said it was time to go back to my primary care doctor and any further medication would have to be prescribed by her.
I went to see her, but she still did not feel comfortable handling my care and referred me to a pain clinic 6 hours away. I was in despair, thinking that I had crippled myself for life and would lose my job, my son and my husband. All of these relationships were strained at this point.
The pain clinic helped me get my life back. They are compassionate and good to the people that come through their doors. It’s a common misconception that pain patients want to take medication. We don’t. We just want some of our lives back and pain medication helps us have that.
A year after my fusion, the surgeon met me again. The fusion had failed, and he wanted to do a revision that would be more painful than the first. He also told me he thought my pain might be caused by fibromyalgia. I’ve never been so angry. I have pain because of my broken neck. Pompous arrogant doctor with no aftercare.
Here is my dilemma, I’ve gotten better care in a big city, where they do not treat me like an addict. I’ve gotten my life back. At first, I was able to go there every three months to get my medication, but with the laws changing, they now say I have to go every month. Driving 6 hours both ways with a 5-year-old and a broken neck is hard. But quality of life and pain are great motivators.
My experience has left me with so much anger towards doctors in my area. It seems their Hippocratic oath has been trumped by the opioid crisis and fear of administrative action. I do not tell people about the medication that helps my quality of life for fear of judgement and stigma. Unless they have been through chronic pain, they simply don’t understand.
I wouldn’t wish this on my worst enemy.
Bailey Parker lives in Colorado.
Pain News Network invites other readers to share their stories with us. Send them to editor@painnewsnetwork.org.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.