Why Exercise Should Be Your First Treatment for Osteoarthritis
/By Clodagh Toomey
Stiff knees, aching hips and the slow grind of chronic joint pain are often accepted as an unavoidable part of getting older. But while osteoarthritis is the world’s most common joint disease, experts say the way we treat and prevent it is badly out of step with the evidence.
The best medicine isn’t found in a pill bottle or an operating theatre – it’s movement. Yet across countries and health systems, too few patients are being guided toward the one therapy proven to protect their joints and ease their pain: exercise.
Exercise is one of the most effective treatments for chronic, disabling joint conditions such as osteoarthritis. Yet very few patients actually receive it.
Research across health systems in Ireland, the UK, Norway and the United States shows the same pattern: fewer than half of people with osteoarthritis are referred to exercise or physiotherapy by their primary care provider. More than 60% are given treatments that guidelines do not recommend, and around 40% are sent to a surgeon before non-surgical options have even been tried.
To understand why those figures are so troubling, it helps to understand what exercise does for joints. Osteoarthritis is by far the most common form of arthritis, already affecting more than 595 million people worldwide.
According to a global study in The Lancet, that number could approach one billion by 2050. Longer life expectancy, increasingly sedentary lifestyles and rising numbers of overweight or obese people are driving the trend.
Yet people who exercise regularly are physically and biologically protecting themselves from developing the disease and from suffering its worst effects.
The cartilage that covers the ends of our bones is a tough, protective layer with no blood supply of its own. It relies on movement.
Like a sponge, cartilage is compressed when we walk or load a joint, squeezing fluid out and then drawing fresh nutrients back in. Each step allows nutrients and natural lubricants to circulate and maintain joint health.
That is why the old idea of osteoarthritis as simple “wear and tear” is misleading. Joints are not car tires that inevitably grind down.
Osteoarthritis is better understood as a long process of wear and repair in which regular movement and exercise are critical to healing and to the health of the entire joint.
A Disease of the Whole Joint
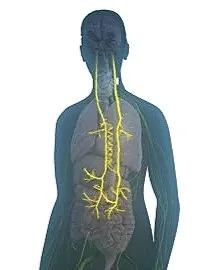
We now know osteoarthritis is a whole-joint disease. It affects the joint fluid, the underlying bone, the ligaments, the surrounding muscles and even the nerves that support movement.
Therapeutic exercise targets all these elements. Muscle weakness, for instance, is one of the earliest signs of osteoarthritis and can be improved with resistance training. There is strong evidence that muscle weakness increases the risk of both developing the disease and seeing it progress.
Nerve and muscle control can also be trained through neuromuscular exercise programmes such as GLA:D® (Good Life with osteoArthritis: Denmark) for hip and knee osteoarthritis. Usually delivered in supervised group sessions by physiotherapists, these programmes focus on movement quality, balance and strength to improve joint stability and rebuild confidence.
Significant improvements in pain, joint function and quality of life have been recorded for up to 12 months after completing the programme.
Exercise is good medicine for the whole body: it has documented benefits across more than 26 chronic diseases. In osteoarthritis, it helps not only by strengthening cartilage and muscle but also by tackling the inflammation, metabolic changes and hormonal shifts that drive the disease.
Obesity is a major risk factor for osteoarthritis, and not merely because of the extra mechanical load on joints. High levels of inflammatory molecules in the blood and in joint tissues can degrade cartilage and accelerate disease.
For osteoarthritis, regular activity can counter this at a molecular level, lowering inflammatory markers, limiting cell damage and even altering gene expression.
Exercise First, Surgery Later
Currently there are no drugs that modify the course of osteoarthritis. Joint replacement surgery can be life-changing for some people, but it is major surgery and does not succeed for everyone.
Exercise should be tried first and continued throughout every stage of the disease. It carries far fewer side effects and brings many additional health benefits.
Osteoarthritis is not simply a matter of “worn out” joints. It is shaped by muscle strength, inflammation, metabolism and lifestyle.
Regular, targeted exercise addresses many of these factors at once – helping to protect cartilage, strengthen the whole joint and improve overall health. Before considering surgery, movement itself remains one of the most powerful treatments we have.
Clodagh Toomey, PhD, is a Physiotherapist and Associate Professor in the School of Allied Health at the University of Limerick in Ireland.
This article originally appeared in The Conversation and is republished with permission.