Unnecessary Back Surgeries Performed Every 8 Minutes at U.S. Hospitals
/By Pat Anson
Over 200,000 unnecessary or “low value” back surgeries have been performed on older patients at U.S. hospitals over the last three years, about one procedure every eight minutes, according to a new report.
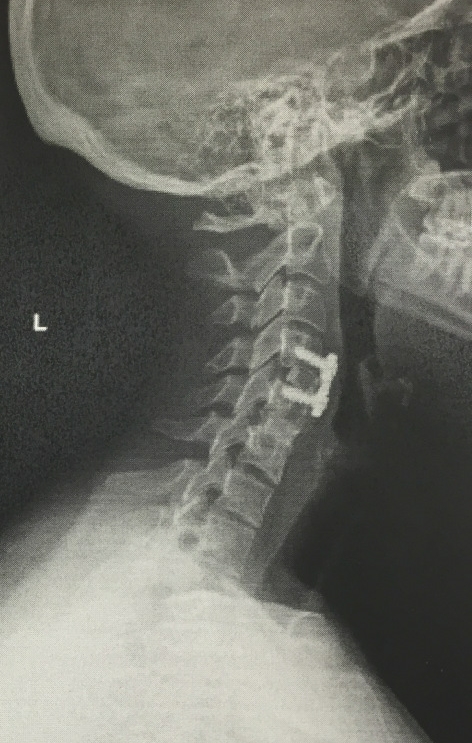
The analysis by the Lown Institute estimates the potential cost to Medicare at $2 billion for unnecessary spinal fusions, laminectomies and vertebroplasties. The procedures either fuse vertebrae together, remove part of a vertebra (laminectomy), or inject bone-like cement into fractured vertebrae (vertebroplasty) to stabilize them.
Lown maintains that fusions and laminectomies have little or no benefit for low-back pain caused by aging, while patients with spinal fractures caused by osteoporosis receive little benefit from vertebroplasties.
“We trust that our doctors make decisions based on the best available evidence, but that’s not always the case,” said Vikas Saini, MD, president of the Lown Institute, an independent think tank that analyzed Medicare and Medicare Advantage claims from 2019 to 2022.
“In spinal surgery, as with other fields of medicine, physicians routinely overlook evidence to make exceptions, sometimes at shockingly high rates. This type of waste in Medicare is costly, both in terms of spending, and in risk to patients.”
Up to 30 million Americans receive medical care for spine problems each year. While surgery is appropriate for some, the Lown Institute considers many common surgeries overused and of low value to patients. Potential risks include infection, blood clots, stroke, heart and lung problems, paralysis and even death.
Spinal fusions and laminectomies are considered useful for patients who have low back pain caused by trauma, herniated discs, discitis, spondylosis, myelopathy, radiculopathy and scoliosis. Fusions are also appropriate for patients with spinal stenosis from neural claudication and spondylolisthesis; and laminectomies are appropriate for patients with stenosis who have neural claudication.
Wide Variation in Overuse Rates
Nationwide, about 14% of spinal fusions/laminectomies met the criteria for overuse, while 11% of surgery patients with osteoporosis received an unnecessary vertebroplasty.
The Lown Institute found a wide variation in overuse rates at some of the nation’s largest and most prestigious hospitals. UC San Diego, for example, had a 1.2% overuse rate for fusions and laminectomies; while the Hospital of the University of Pennsylvania had a 32.6% overuse rate.
The largest overuse rate was at Mt. Nittany Medical Center in Pennsylvania, where nearly two-thirds (62.8%) of the fusions and laminectomies were considered inappropriate or of low value.
The Lown report found that over 3,400 doctors performed a high number of low-value back surgeries. Those physicians received a total of $64 million from device and drug companies for consulting, speaking fees, meals and travel, according to Open Payments. Three companies — Nuvasive, Medtronic and Stryker — paid over $22 million to doctors who performed the unnecessary surgeries.
Previous reports by the Lown Institute have also questioned the value of procedures such as knee arthroscopies, a type of “keyhole” surgery in which a small incision is made in the knee to repair ligaments. Research has found that arthroscopic surgeries provide only temporary relief from knee pain and do not improve function long-term.
The American Hospital Association takes a dim view of Lown studies, calling the data cherry-picked and misleading.