Limiting Rx Opioids Is Making Opioid Epidemic Worse
/By David Hanscom, MD, PNN Columnist
I am an orthopedic spine surgeon who specializes in complex problems in all areas of the spinal column.
Over the last five years, a significant percent of my practice has been addressing spine infections, most of them in patients addicted to intravenous drugs. Bacteria can enter the blood stream from a contaminated needle and lodge in the discs between the vertebrae, which have a limited blood supply. It’s an ideal environment for bacterial growth and it destroys the neighboring discs and vertebra. Often they weaken to the point where they break.
Corrective surgery entails draining the infection and then stabilizing the broken spine with a fusion. These operations are complex, expensive and risky. After surgery there is a minimum of six weeks of IV antibiotics. Occasionally, a patient ends up paralyzed because the infection cuts off the blood supply to the spinal cord.
One typical case was that of middle-aged carpenter with low back pain, who had been able to work for years by taking a stable low dose of opioid medication. He needed to keep working, so when the local pain clinic shut down, he felt he had no other choice but to use IV heroin. His spine became infected and the infection spread deeply into his pelvis. I met him in the hospital when he was extremely ill, and it took three operations to drain and stabilize his spine.
My experience from this and other cases tells me the opioid epidemic is rapidly getting worse. In addition to the medical problems created from IV drug abuse, there were nearly 49,000 overdose deaths from opioids – both legal and illegal -- in 2017. Unfortunately, there doesn’t appear to be a viable solution in sight. In fact, current efforts to reduce opioid prescribing are exacerbating the problem. Although I agree with more careful prescribing practices, it isn’t the answer to the epidemic.
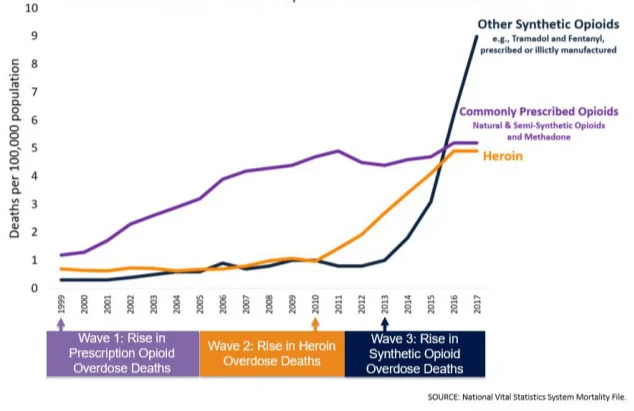
This CDC graphic tells why. As deaths from prescription opioids leveled off over the past several years, mortality from heroin and synthetic opioids like illicit fentanyl have spiked higher. Although the medical system is decreasing the supply of prescription opioids, it’s pushing people to these illicit sources.
Chronic Pain and Anxiety
Nearly 90 percent of patients on opioids have chronic pain, while the rest mostly suffer from acute pain. But the mental pain is a far greater problem than the physical pain. Any physical or mental threat causes your body to secrete stress hormones, such as cortisol, adrenaline and histamines to improve your chances of survival.
The sensation created by these chemicals is anxiety. Humans have a major problem when they can’t escape from negative thoughts. Anxiety triggers a sustained chemical assault that we will try almost anything to escape from. This unconscious and automatic survival response is over a million times stronger than the conscious brain.
Research has documented that when you are upset for any reason, your pain will increase. It isn’t psychological or “all in your head.” There’s a direct linkage between pain circuits and stress. You will experience an increased speed of nerve conduction from stress chemicals, causing your pain levels to increase.
Many Treatments Don’t Work
Another problem is that modern medicine isn’t providing viable solutions to chronic pain. A recent survey found that only about 1% of physicians enjoy and are comfortable treating chronic pain.
Modern medicine is only pretending to treat your pain. You go to the doctor trusting him or her to help you and you’re repeatedly disappointed. As your frustration grows, your stress hormones remain elevated and your pain physically worsens.
Even worse, many “mainstream” interventions such as surgery have been demonstrated to be ineffective and often cause harm, while effective treatments are not readily available because they are not covered by insurance. A significant percent of a medical system’s revenue is driven by these expensive and risky interventions.
Instead of exploring ways to implement effective treatments for pain, the government and medical establishment are focusing their efforts on restricting access to pain medications -- with most of the focus being on the providers. Physicians are now afraid to prescribe long-term opioids, even though most of us have had patients thrive on a stable opioid regimen.
This is the worst step that could be taken because patients immediately experience increased anxiety, frustration and eventually anger when they are cutoff or have their doses reduced.
What can we do to solve the opioid epidemic?
First, solve chronic pain! Recent medical research has revealed possible solutions but mainstream medicine isn’t implementing them.
Second, recognize that what drives most people to use opioids is mental pain. Physical pain is often secondary.
Third, environmental factors, especially family dynamics may be exacerbating chronic pain. Allow physicians to take the time to listen to patients and focus on their real problems, rather than just randomly treat their symptoms.
Finally, since the problem is so pervasive, the answers must be widely available and implemented by anyone.
Dr. David Hanscom is a spinal surgeon who has helped hundreds of back pain sufferers by teaching them how to calm their central nervous systems without the use of drugs or surgery.
In his book Back in Control, Hanscom shares the latest developments in neuroscience research and his own personal history with pain.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.