Lyrica Fails in Sciatica Pain Study
/By Pat Anson, Editor
A small study in Australia has found that pregabalin – a drug more widely known under the brand name Lyrica -- works no better than a placebo at relieving leg pain caused by sciatica.
Researchers enrolled 209 sciatica patients in the study and assigned them to groups that received either pregabalin or placebo for a year. The findings, published in the New England Journal of Medicine, not only showed that pregabalin was no more effective than a placebo, but that it caused unwanted side effects such as dizziness.
“Treatment with pregabalin did not significantly reduce the intensity of leg pain associated with sciatica and did not significantly improve other outcomes, as compared with placebo, over the course of 8 weeks. The incidence of adverse events was significantly higher in the pregabalin group than in the placebo group,” researchers concluded.
In all, 227 side effects were reported by the 108 patients who received pregabalin.
"Until now there has been no high quality evidence to help patients and doctors know whether pregabalin works for treating sciatica. Our results have shown pregabalin treatment did not relieve pain, but did cause side effects such as dizziness," said lead author Dr. Christine Lin, an associate professor at the George Institute for Global Health and the University of Sydney Medical School.
The placebo effect appeared to play a strong role in the study. Participants started out with an average score of about 6 on a zero to 10 pain scale. After one year, the pain levels dropped to 3.4 for those taking pregabalin and 3.0 for those taking placebo.
“It seems people associate a drop in pain being due to taking a capsule, rather than something which would happen naturally over time,” said Lin. "Unfortunately there are no drugs proven to work for people with sciatica and even epidural injections only provide a small benefit in the short term. What we do know is that most people with sciatica do eventually recover with time. It's also important to avoid bed rest and to stay as active as possible."
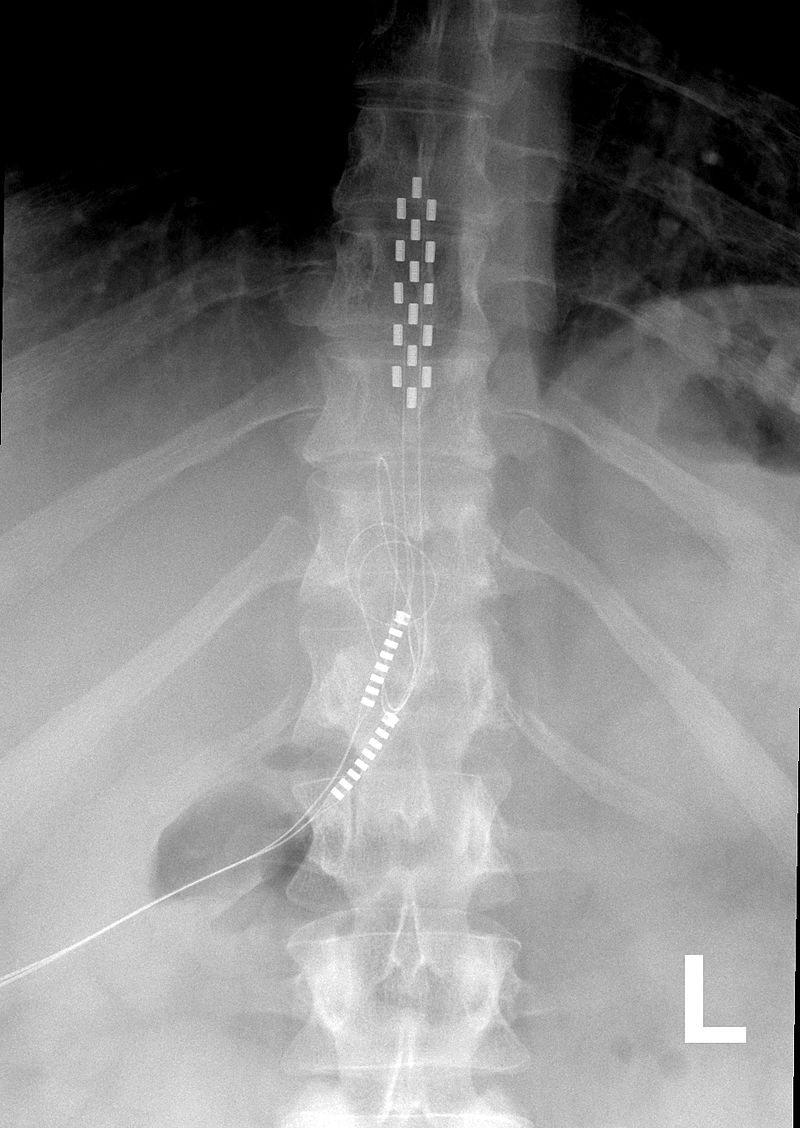
Sciatica originates in the lower back and travels down the sciatic nerve to each leg, causing pain, tingling and numbness.
Pregabalin was originally developed as a treatment for epilepsy, but drug maker Pfizer was very successful in turning Lyrica into a multi-purpose pain drug that generates worldwide sales of $5 billion a year.
The U.S. Food and Drug Administration has approved Lyrica to treat chronic nerve pain caused by diabetes, fibromyalgia, epilepsy, spinal cord injury and post-herpetic neuralgia caused by shingles. The drug is also prescribed “off label” to treat a variety of other conditions, including sciatica and spinal stenosis.
According to ClinicalTrials.gov, dozens of studies are underway to test the effectiveness of pregabalin on conditions such as cirrhosis of the liver, anxiety, chronic cough, post-operative pain, pediatric seizures, and neuropathic pain caused by chemotherapy.
Common side effects of Lyrica are dizziness, blurred vision, nausea, headache, weight gain and fatigue. Lyrica may cause suicidal thoughts in about 1 in 500 patients who use it. Pfizer also warns patients to talk to their doctor before they stop taking Lyrica. Suddenly stopping the medication may result in withdrawal symptoms such as headaches, nausea, diarrhea, trouble sleeping, increased sweating, and anxiety.