Quell Device Relieves Variety of Pain Conditions
/By Pat Anson, Editor
A new medical device that uses electrical nerve stimulation was effective in managing chronic pain in patients suffering from arthritis, neuropathy, fibromyalgia and other conditions, according to a small clinical study conducted by NeuroMetrix (NASDAQ: NURO), the device’s manufacturer.
Pain News Network recently featured the Quell Wearable Pain Relief device in a column by J.W. Kain, who reported that Quell “worked brilliantly” in relieving her chronic neck and back pain.
Eighty eight people were enrolled in a 60-day trial of Quell. All had chronic pain for at least year and nearly a quarter had more than 15 years of pain. Participants had “complex medical histories” with arthritis (61%), diabetic nerve pain (40%), sciatica (27%), and fibromyalgia (26%) as the most common conditions.
Over 80 percent of the participants said Quell relieved their chronic pain and improved their overall health. The largest measured changes were in pain relief, along with improved sleep, general activity, and walking ability.
Over two-thirds of the patients said Quell also reduced the amount of pain medication they were taking
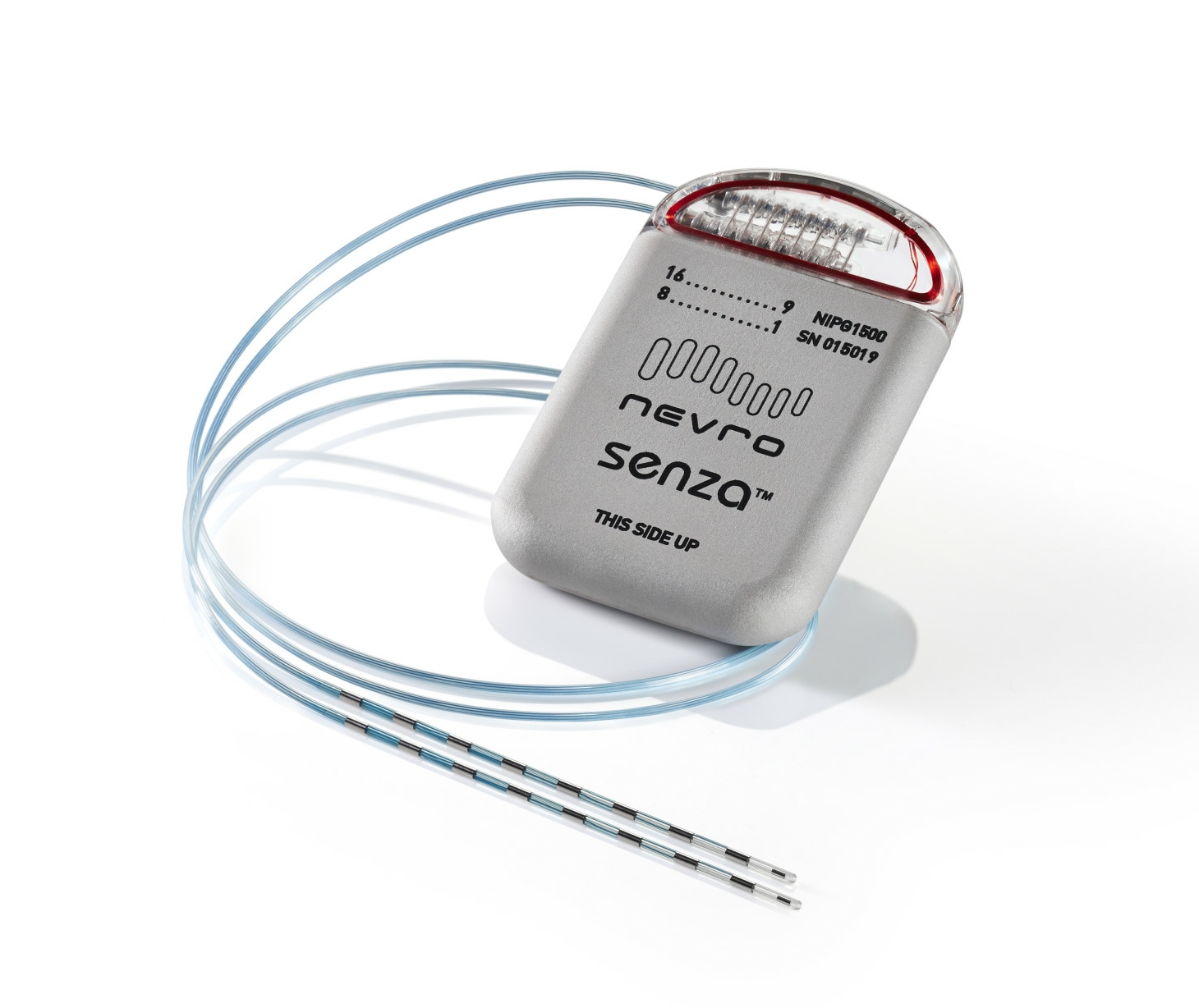
image courtesy of neurometrix
"We are pleased with these results. They represent the first formal evaluation of self-administered wearable intensive nerve stimulation. Quell provided substantial pain relief and improvement in quality of life measures,” said Shai N. Gozani, MD, President and CEO of NeuroMetrix.
“We were not surprised that two-thirds of the subjects reduced their use of pain medications, as we have consistently received this anecdotal feedback from Quell users over the past several months.”
Quell is available over-the-counter and does not require a prescription. It relieves pain by using electric stimulation to “mask” pain signals before they reach brain, much like a TENS unit. The device, which costs $249, is lightweight and designed to be worn over the upper calf during the day or night.
The marketing of Quell for the treatment of chronic pain was approved by the Food and Drug Administration in 2014, but NeuroMatrix did not begin shipping the device to healthcare providers until this summer. It is also available through the company’s website.
A study abstract, “Treatment of Chronic Pain with a Novel Wearable Transcutaneous Electrical Nerve Stimulator,” has been accepted for poster presentation at the annual PAINWeek conference next month in Las Vegas.