Should Pain Patients Be Prescribed Naloxone?
/By Pat Anson, Editor
A medication that rapidly reverses the effects of an opioid overdose should be prescribed to patients taking opioid analgesics for chronic pain, according to a study published in the Annals of Internal Medicine.
But the study fails to address the soaring cost of naloxone and whether pain patients can afford it.
In a pilot program at primary care clinics in San Francisco, doctors gave naloxone “rescue kits” to nearly 2,000 pain patients on long-term opioid therapy, and found that they had 63 percent fewer opioid-related emergency rooms visits in one year than patients not prescribed naloxone. Naloxone is usually administered by injection to reverse the effects of an overdose and has been credited with saving thousands of lives.
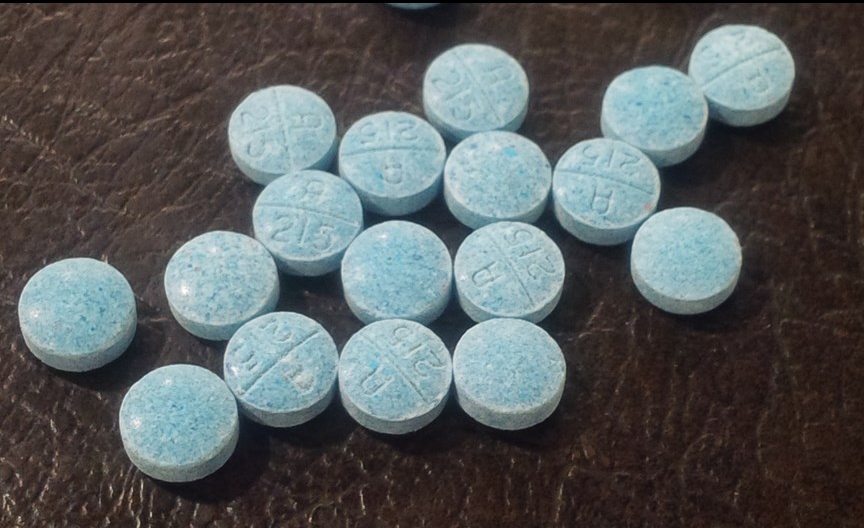
Naloxone has rapidly gone mainstream in recent years as public health officials have reacted to the so-called opioid epidemic. The rescue kits are increasingly being carried by police and paramedics, and given to heroin and opioid addicts to keep at home. But they are not usually prescribed to people taking opioids for pain relief.
Researchers say being given a rescue kit and being trained how to use one may have made pain patients in the study more careful with their opioids, without the kits ever actually being used.
“The educational component of the intervention may have reduced ED (emergency department) visits by altering risky behaviors, thus preventing overdoses in the first place,” said lead author Alexander Walley, MD, in an editorial also published in the Annals of Internal Medicine. "Receiving a naloxone rescue kit may have served as tangible reinforcement of overdose prevention messages, though this warrants further study.”
university of washington
The Centers for Disease Control and Prevention recently released opioid prescribing guidelines that encourage physicians to prescribe naloxone to high-risk patients.
“Providers should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, or higher opioid dosages (≥50 MME), are present,” the guidelines state.
The Food and Drug Administration is also encouraging the widespread distribution of naloxone. Last November, the agency approved Narcan -- a naloxone nasal spray – as an emergency life-saving medication. The approval came less than four months after the FDA received a new drug application from Adept Pharma. The process usually take the agency years to complete.
“Anyone who uses prescription opioids for the long term management of chronic pain, or those who take heroin, are potentially at risk of experiencing a life-threatening or fatal opioid overdose where breathing and heart beat slow or stop,” Adept Pharma said in a statement.
The company said Narcan would be available at a “public interest price” of $75 for a package of two nasal sprays when ordered by public health organizations. For consumers, however, Narcan costs nearly twice as much. Healthcare Bluebook lists the retail “fair price” of Narcan at $134.
Prices for naloxone have soared in recent years as demand for the medication has increased. Some hospital emergency departments have run out of naloxone, according to Politico, and some drug makers are being accused of price gouging.
"You have increased demand and a few people who control the pricing, so they can charge whatever they want," said Eliza Wheeler, who runs an overdose prevention project in Northern California, in Politico.
Generic versions of naloxone cost only pennies in other countries, but in the U.S. an auto inject version sold by Kaleo Pharma soared from $575 for a two-dose package to $3,750, according to Truven Health Analytics.
“Opioid abuse is an epidemic across our country, yet drug companies continue to rip off the American people by charging the highest prices in the world because they have no shame,” Democratic presidential candidate Sen. Bernie Sanders said in a statement. “The greed of the pharmaceutical industry is killing Americans.”
Many drug makers offer discounts on naloxone rescue kits to hospitals, schools, non-profits and public agencies, but patients often wind up paying full price.