How CDC Bungled Early Coronavirus Testing
/By Rachana Pradhan, Kaiser Health News
As the novel coronavirus snaked its way across the globe, the Centers for Disease Control and Prevention in early February distributed 200 test kits it had produced to more than 100 public health labs run by states and counties nationwide.
Each kit contained material to test a mere 300 to 400 patients. And labs, whether serving the population of New York City or tiny towns in rural America, apparently received the same kits.
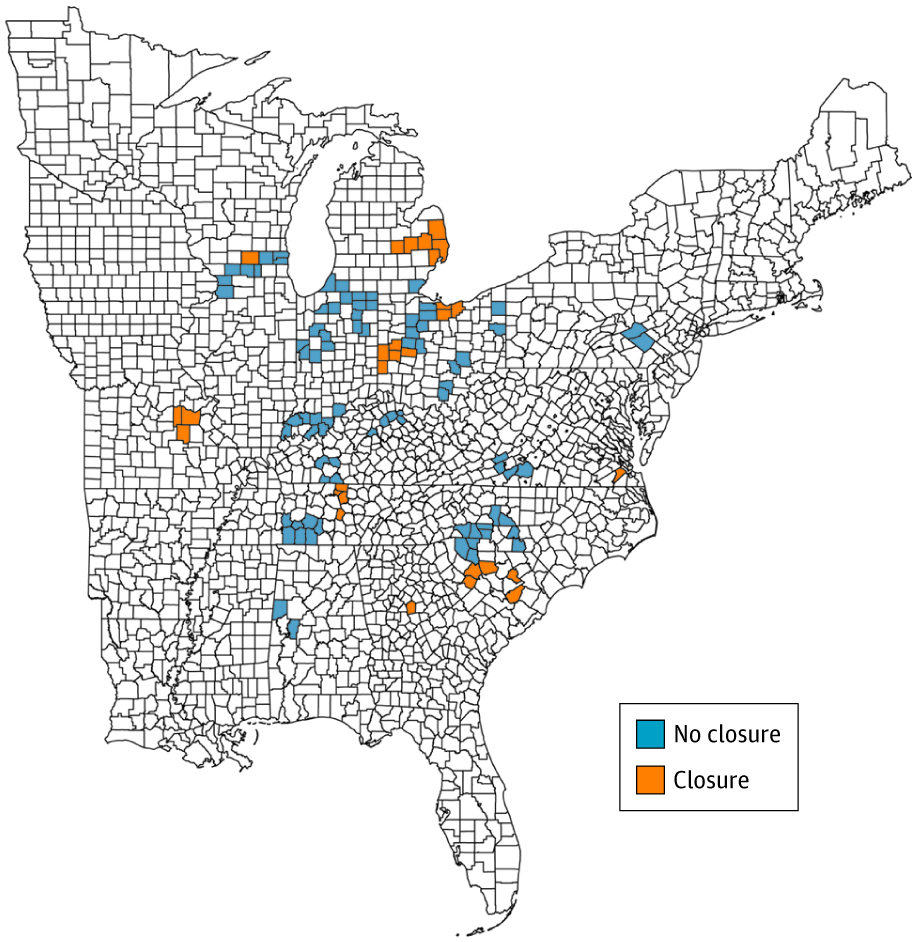
The kits were distributed roughly equally to locales in all 50 states. That decision presaged weeks of chaos, in which the availability of COVID-19 tests seemed oddly out of sync with where testing was needed.
A woman in South Dakota with mild symptoms and no fever readily got the test and the results. Meanwhile, political leaders and public officials in places like New York, Boston, Seattle and the San Francisco Bay Area — all in the throes of serious outbreaks ― couldn’t get enough tests to screen ill patients or, thereby, the information they needed to protect the general public and stem the outbreak of the virus, whose symptoms mimic those of common respiratory illnesses.
Rapid testing is crucial in the early stages of an outbreak. It allows health workers and families to identify and focus on treating those infected and isolate them.
Yet health officials in New York City and such states as New York, Washington, Pennsylvania and Georgia confirmed to Kaiser Health News that they each initially got one test kit, calling into question whether they would have even stood a chance to contain the outbreaks that would emerge. They would soon discover that the tests they did receive were flawed, lacking critical components and delivering faulty results.
During those early weeks, the virus took off, infecting thousands of people and leading to nationwide social distancing and sheltering in place. Public health officials are just beginning to grapple with the fallout from that early bungling of testing, which is likely to haunt the country in the months to come.
Too Little Too Late
The first shipment to Washington state arrived more than two weeks after officials there announced the first U.S. case of coronavirus, and at a moment when deadly outbreaks of the disease were already festering in places like the Life Care Center in Kirkland. Within weeks, three dozen people infected with COVID-19 would die at the nursing home in the suburbs of Seattle.
The spread of COVID19 would not take long to overwhelm the state, which has over 2,200 people infected.
The Trump administration in recent days has attempted to speed testing for the virus after early missteps hampered the government’s response to contain the contagion, and officials have had to respond to a barrage of criticism from public health experts, state officials and members of Congress.
Federal health officials have eased the process for university and commercial labs to perform their own tests, and they are ramping up their capacity. As of March 16, public and private labs in the U.S. had the ability to test more than 36,000 people a day, according to estimates compiled by the American Enterprise Institute, a conservative-leaning think tank in Washington, D.C., a figure expected to rapidly escalate in coming weeks. That figure, however, can vary considerably by state and does not indicate how many tests are actually given to patients.
“We are now beginning to see that they have spread out in a prioritized way. We asked them to prioritize the regions that were mostly affected,” Deborah Birx, the coronavirus response coordinator for the White House Coronavirus Task Force, said Wednesday of private labs’ testing, without elaboration.
The scaling up of testing is set to take place after weeks of faltering and hundreds, if not thousands, of undiagnosed people spreading the virus. For example, New York’s state health department received a faulty CDC test kit on Feb. 8 for 800 patient specimens, an amount that’s consistent with other states, according to a spokesperson. It later began testing patients with a test that state officials developed based on the CDC protocol and has significantly increased testing.
In New York City, the first batch was obtained on Feb. 7.
“The other state and local public health laboratories got test kits as they became available,” said Eric Blank, chief program officer of the Association of Public Health Laboratories.
Places in the middle of the country with no outbreaks had the luxury of time to plan. For example, Missouri officials have had about 800 tests to work with, leading to only 395 performed so far in the region by public health labs ― 26 of which were positive. When private lab tests are accounted for, as of Friday there were 47 confirmed cases.
Health care providers and public health staff in the state, however, benefited from the fact that there is less international travel to the region, according to infectious disease expert Dr. Steven Lawrence of Washington University in St. Louis.
“This is very similar to 1918 with the influenza pandemic — St. Louis had more time to prepare and was able to put measures in place to flatten the curve than, say, Philadelphia,” Lawrence said. “Seattle didn’t have an opportunity to prepare as much in advance.”
While commercial labs are coming online, strict restrictions are limiting testing capabilities, Lawrence said.
“The state has had their hands tied,” he added.
Waiting and Wondering
Because of a widespread lag in testing, it is still a mystery for thousands of people to know whether they’ve come into contact with an infected person until well after it happens.
“CDC will distribute tests based on where they can do the most good. But without hospital-based testing and commercial testing, it will not be possible to meet the need,” said Tom Frieden, who led the CDC during the Obama administration and is a former commissioner of the New York City Health Department.
Since the CDC’s initial distribution, states have been reordering more tests through the office’s International Reagent Resource ― a long-standing tool that public health labs have relied on. They have also revised testing protocols to use only one sample per person, which boosts the number of people screened.
Yet problems still abound with tests or other materials needed to be able to detect the virus. California Gov. Gavin Newsom said on March 12 that county public health labs can’t use all of the 8,000 test kits the state has because they are missing key components.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation, which is not affiliated with Kaiser Permanente.