The Prescription Opioid Crisis Is Over
/By Roger Chriss, PNN Columnist
In a very real sense, the prescription opioid crisis is over. But it didn’t end and we didn’t win. Instead, it has evolved into a broader drug overdose crisis. Opioids are still a factor, but so is almost every other class of drug, whether prescribed or sourced on the street.
The main players in the crisis now are illicit fentanyl, cocaine and methamphetamine. The vast majority of fatal overdoses include a mixture of these drugs, with alcohol and cannabis often present, and assigning any one as the sole cause of death is becoming tricky.
Connecticut Magazine recently reported on rising fentanyl overdoses in that state. According to the Office of the Chief Medical Examiner, fentanyl deaths in Connecticut spiked from 14 in 2012 to 760 in 2018. Fentanyl was involved in 75% of all overdoses last year, often in combination with other drugs
Meanwhile, overdoses involving the most widely prescribed opioid — oxycodone — fell to just 62 deaths, the lowest in years. Only about 6% of the overdoses in Connecticut were linked to oxycodone.
Similar trends can be seen nationwide, mostly east of the Mississippi. Opioids still play a major role in drug deaths, with the CDC reporting that about 68% of 70,200 drug overdose deaths in 2017 involving an opioid. But more than half of these deaths involved fentanyl and other synthetic opioids obtained on the black market.
According to the National Institute on Drug Abuse, overdoses involving prescription opioids or heroin have plateaued, while overdoses involving methamphetamine, cocaine and benzodiazepines have risen sharply.
In other words, deaths attributable to prescription opioids alone are in decline. Deaths attributable to fentanyl are spiking, and deaths involving most other drug class are rising rapidly. The CDC estimates that there are now more overdoses involving cocaine than prescription opioids or heroin.
Moreover, the crisis is evolving fast. At the American College of Medical Toxicology’s 2019 annual meeting, featured speaker Keith Humphreys, PhD, remarked that “Fentanyl was invented in the sixties. To get to 10,000 deaths took 50 years. To get to 20,000 took 12 months.”
In fact, provisional estimates from the CDC for 2018 suggest we have reached 30,000 fentanyl deaths. And state-level data show few signs of improvements for 2019.
Worryingly, methamphetamine use is resurgent. And cocaine is “making a deadly return.” Illicit drugs are also being mixed together in novel ways, with “fentanyl speedballs” – a mixture of fentanyl with cocaine or meth – being one example.
Drug Strategies ‘Need to Evolve’
The over-emphasis on prescription opioids in the overdose crisis has led to an under-appreciation of these broader drug trends. Researchers are seeing a need for this to change.
“The rise in deaths involving cocaine and psychostimulants and the continuing evolution of the drug landscape indicate a need for a rapid, multifaceted, and broad approach that includes more timely and comprehensive surveillance efforts to inform tailored and effective prevention and response strategies,” CDC researchers reported last week. “Because some stimulant deaths are also increasing without opioid co-involvement, prevention and response strategies need to evolve accordingly.”
It is now common to hear about the “biopsychosocial” model for treating chronic pain – understanding the complex interaction between human biology, psychology and social factors. This same model has a lot to offer substance use and drug policy.
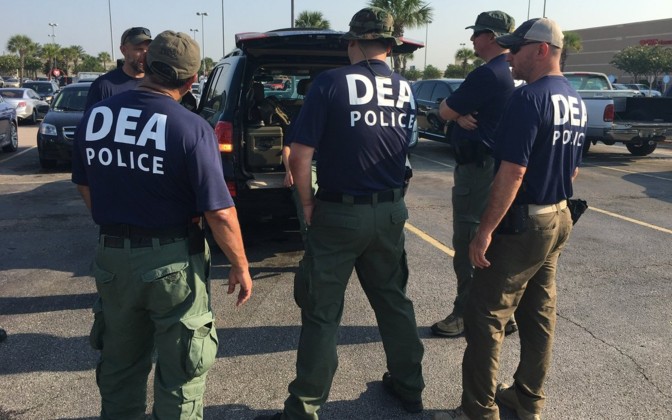
Substance use and addiction involve a complex interplay of genetic and epigenetic factors combined with social and cultural determinants. Treatment must be more than just saying no or interdicting suppliers. At present, medication-assisted therapy for opioid use disorder remains hard to access. And other forms of addiction have no known pharmacological treatment.
Addressing the drug overdose crisis will require not only more and better treatment but also increased efforts at harm reduction, decriminalization of drug use, improvements in healthcare, and better public health surveillance and epidemiological monitoring. Further, the underlying social and cultural factors that make American culture so vulnerable to addiction must be addressed.
None of this is going to be easy. Current efforts are misdirected, making America feel helpless and look hapless. Novel and possibly disruptive options may prove useful, from treating addiction with psychedelics to reducing risks of drug use through safe injection sites and clean needle exchanges.
We are long past the prescription opioid phase of the crisis, and are now in what is variously being called a “stimulant phase” and a “poly-drug phase.” Recognition of the shape of the drug overdose crisis is an essential first step toward changing its grim trajectory.
Roger Chriss lives with Ehlers Danlos syndrome and is a proud member of the Ehlers-Danlos Society. Roger is a technical consultant in Washington state, where he specializes in mathematics and research.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.