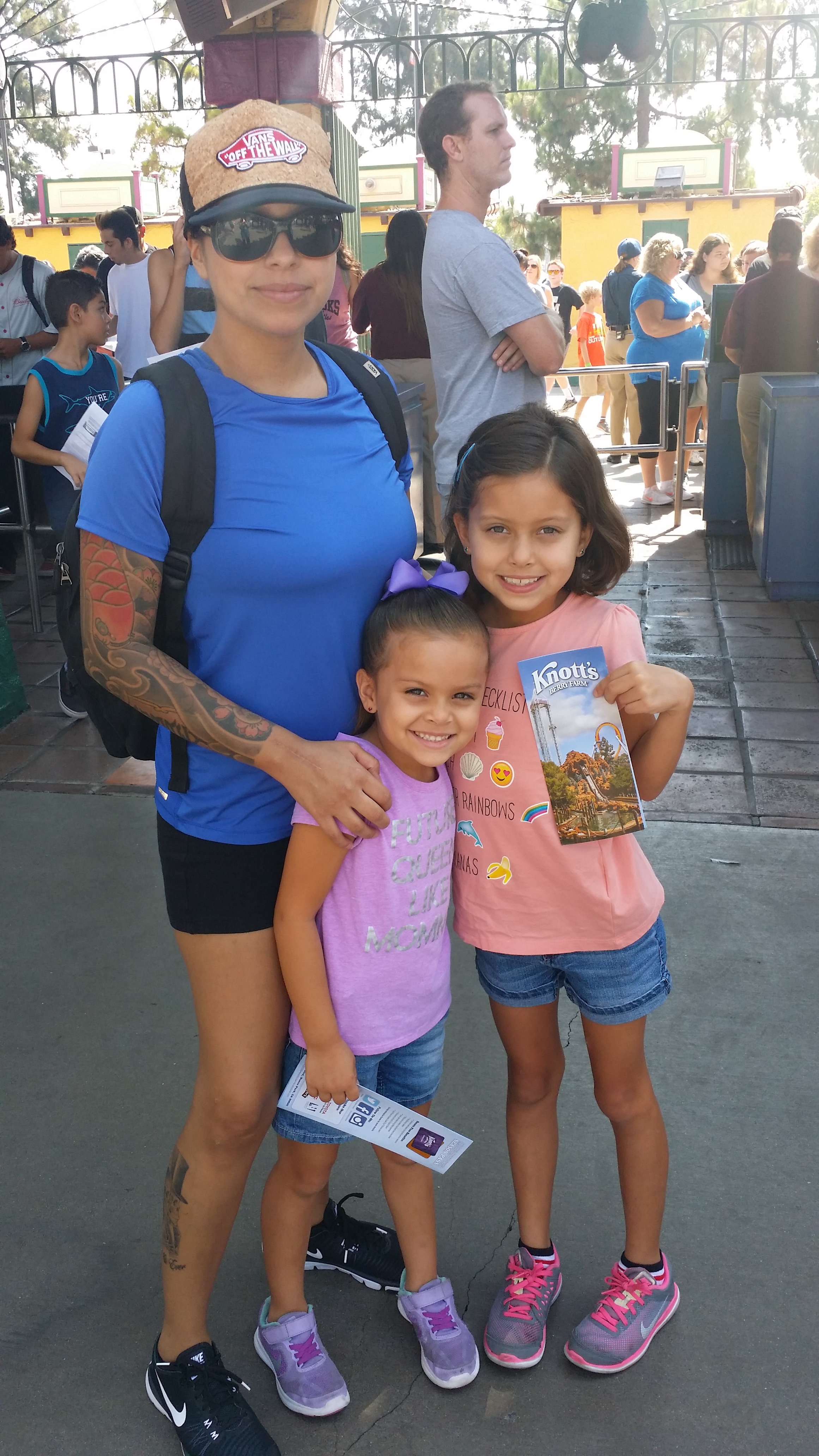
Miss Understood: A Mother’s Greatest Fear
/By Arlene Grau, Columnist
As a mother your main goals are to raise your children to lead happy lives, to always love them, and to keep them safe. I want to see my children excel and get a lot further in life than anything I've ever dreamed of.
Although I have many hopes and aspirations for my two daughters, my worst fear is always lingering in the back of my head.
What if I cursed one of my daughters with a genetic predisposition for an autoimmune disease? What if they develop arthritis or lupus? I could never forgive myself if I knew they were meant to endure the suffering I've lived through.
I would give anything if they would never have to worry about seeing a medical specialist, or needing infusions, blood draws and painkillers just to get by. They already see a pain sufferer’s life through a child’s point of view and that alone is very difficult to handle for a 5 and 9-year old. But burdening them with this lifestyle would be cruel in and of itself.
I'd like to think that I could handle any amount of pain you throw at me. I'll shed some tears and break down a bit, but I think of myself as a genuinely strong individual. However, if you involve my children, then all bets are off and I become vulnerable.
When my oldest daughter was born I suffered from preeclampsia (high blood pressure) and she was born prematurely. She weighed just 4.6 lbs. at birth and was in the neonatal intensive care unit for two weeks.
The day after I was discharged, I was back at her bedside from the time visiting hours began until it was time to go home. She ended up needing surgery at 8 weeks and it was the worst experience I've ever been through.
I can remember how much I wanted both my girls to come home from the hospital with me so I can just love and protect them. My desire for children was always about how much I wanted a family, but I never stopped to think about the possibility of passing down an autoimmune disease. Now anytime my kids tell me their back or hands hurt, I subconsciously think that it might be arthritis.
I think I may always feel that way. Not only because I'm blaming myself for any pain they may be feeling, but because I know that these diseases do not discriminate against any age group.
Arlene Grau lives in southern California with her family. Arlene suffers from rheumatoid arthritis, fibromyalgia, lupus, migraine, vasculitis, and Sjogren’s disease.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represent the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.