NBA Coach Tried Marijuana for Back Pain
/By Pat Anson, Editor
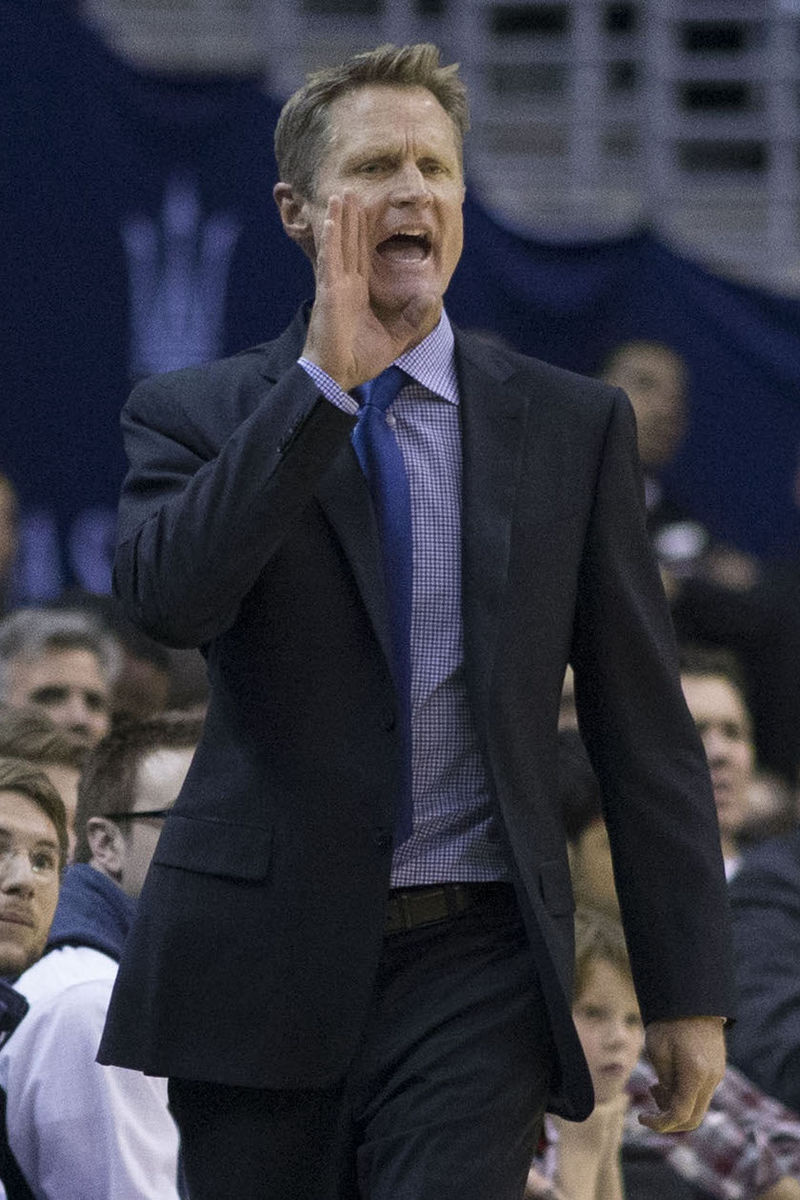
Steve Kerr may have inadvertently started a national conversation about sports and medical marijuana. They’re certainly talking about it in the NBA.
The 51-year old coach of the Golden State Warriors revealed in an interview Friday that he smoked marijuana to see if it might relieve his chronic back pain. Medical marijuana has been legal in California since 1996.
“I guess maybe I can even get in some trouble for this, but I’ve actually tried it twice during the last year and a half, when I’ve been going through this chronic pain that I’ve been dealing with,” Kerr said on The Warriors Insider Podcast.
STEVE KERR
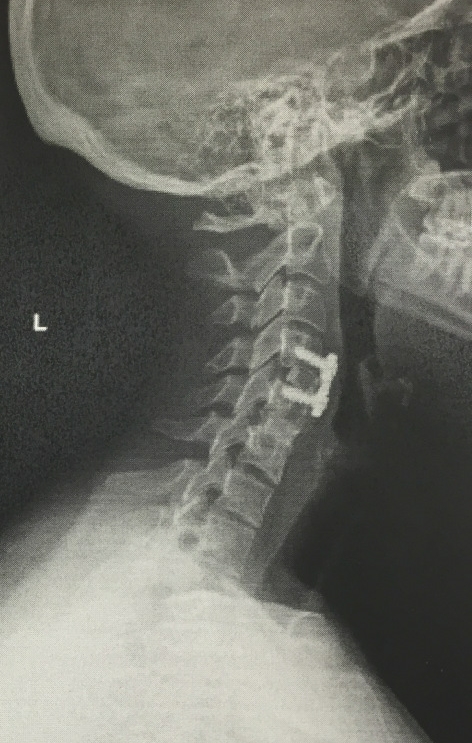
Kerr missed most of the 2015 regular season after two back surgeries that not only failed to relieve his pain, but resulted in a spinal fluid leak that gave him chronic headaches, nausea and neck pain. Kerr took a leave of absence for four months and started trying various pain relievers, including narcotic painkillers and pot.
“A lot of research, a lot of advice from people, and I have no idea if maybe I would have failed a drug test. I don't even know if I'm subject to a drug test or any laws from the NBA, but I tried it and it didn't help it all. But it was worth it because I'm searching for answers on pain. I've tried painkillers and drugs of other kinds as well, and those have been worse. It's tricky," Kerr said.
It’s even trickier if you’re a professional athlete.
If an NBA player is caught using marijuana – either recreationally or medically – the league requires the player to enroll in and complete a substance abuse treatment program.
A second infraction results in a $25,000 fine. The penalties escalate after that, with a third offense resulting in a 5-game suspension, followed by a 10-game suspension for a 4th infraction.
The NFL and Major League Baseball have similar marijuana policies, with baseball players facing the ultimate penalty after a 4th infraction: Banning from the league.
Even though Kerr is a coach now – he had a lengthy career as a player – it took some courage for him to speak so openly about marijuana.
“I’m not a pot person. It doesn’t agree with me. I’ve tried it a few times, and it did not agree with me at all. So I’m not the expert on this stuff,” Kerr said. “But I do know this: If you’re an NFL player, in particular, and you’ve got a lot of pain, I don’t think there is any question that pot is better for your body than Vicodin. And yet athletes everywhere are prescribed Vicodin like its Vitamin C, like it’s no big deal.
“I would hope, especially for these NFL guys, who are basically involved in a car wreck every Sunday – and maybe four days later, the following Thursday, which is another insane thing the NFL does – I would hope that league will come to its senses and institute a different sort of program where they can help these guys get healthier rather than getting hooked on these painkillers.”
Some of Kerr’s player welcomed his comments about a controversial issue.
''Steve's open-minded, and obviously with the way the world's going, if there's anything you can do that's medicinal, people are all for it, especially when there's stuff like Crohn's disease out there, glaucoma, a bunch of stuff, cancer,” said Klay Thompson. “But not recreationally, that should not be of its use ever. There's obviously a medicinal side to it that people are finding out, especially people with really high pain.''
“I think it makes a lot of sense what he said,” said Draymond Green, adding that he has never tried marijuana and “doesn’t really know how it feels.”
“From what I hear from football guys, I think a lot of them do it because of all the pain they go through,” Green said. “It makes a lot sense. It comes from the earth. Any vegetable that comes from the earth, they encourage you to eat it. So I guess it does make a little sense, as opposed to giving someone a manufactured pill. The way some of these pills take the pain away, it can’t be all good for you.”
Although the NFL has a reputation for regular drug testing and watching for signs of drug abuse, some former players say about half the league is currently using marijuana for pain relief. Many grew tired of using painkillers, which one player calls “a scourge in the locker room.”
Steve Kerr says professional sports needs to re-evaluate its relationship with painkillers and marijuana.
“Having gone through my own bout with chronic pain, I know enough about this stuff – Vicodin is not good for you. It’s not,” said Kerr. “It’s way worse for you than pot, especially if you’re looking for a painkiller and you’re talking about medicinal marijuana, the different strains what they’re able to do with it as a pain reliever. And I think it’s only a matter of time before the NBA and NFL and Major League Baseball realize that.”