Trump Budget Cuts Would Further Limit Pain Research
/By Pat Anson, Editor
The Trump administration has proposed another $1.2 billion in budget cuts for the National Institutes of Health (NIH), which experts say could hamper already anemic efforts at developing new treatments for chronic pain. Most of the reductions at NIH would come from research grant funding.
Only about 1 percent of the NIH budget is designated for pain research, even though more Americans suffer from pain than heart disease, diabetes and cancer combined.
The proposed $1.2 billion reduction in this year’s NIH budget is in addition to the $5.8 billion cut the Trump Administration has already proposed for the agency in 2018.
The $7 billion in savings will be used to help pay for an enhanced border wall with Mexico and increased military spending.
The White House Office of Management and Budget says the NIH budget for 2018 “eliminates programs that are duplicative or have limited impact on public health” and would “help focus resources on the highest priority research and training activities.”
"I will be the first one down lobbying against this," said Ann Romney, who suffers from multiple sclerosis and is the wife of former GOP presidential nominee Mitt Romney.
"Nothing comes from nothing. If you don't have that funding, there will be nothing," she told Yahoo News. "There will be no new treatments, there will be no new drug therapies. Progress in medicine will come to a halt."
Pain Research Already Limited
The lack of spending on pain research -- by both the government and the healthcare industry – was a problem long before the Trump administration came out with its budget plans.
In 2012, researchers at Johns Hopkins University estimated that chronic pain costs the U.S. economy up to $635 billion a year in healthcare costs and lost productivity. Yet the NIH spent only $358 million on pain research that year, according to journalist Judy Foreman in her book, “A Nation in Pain.”
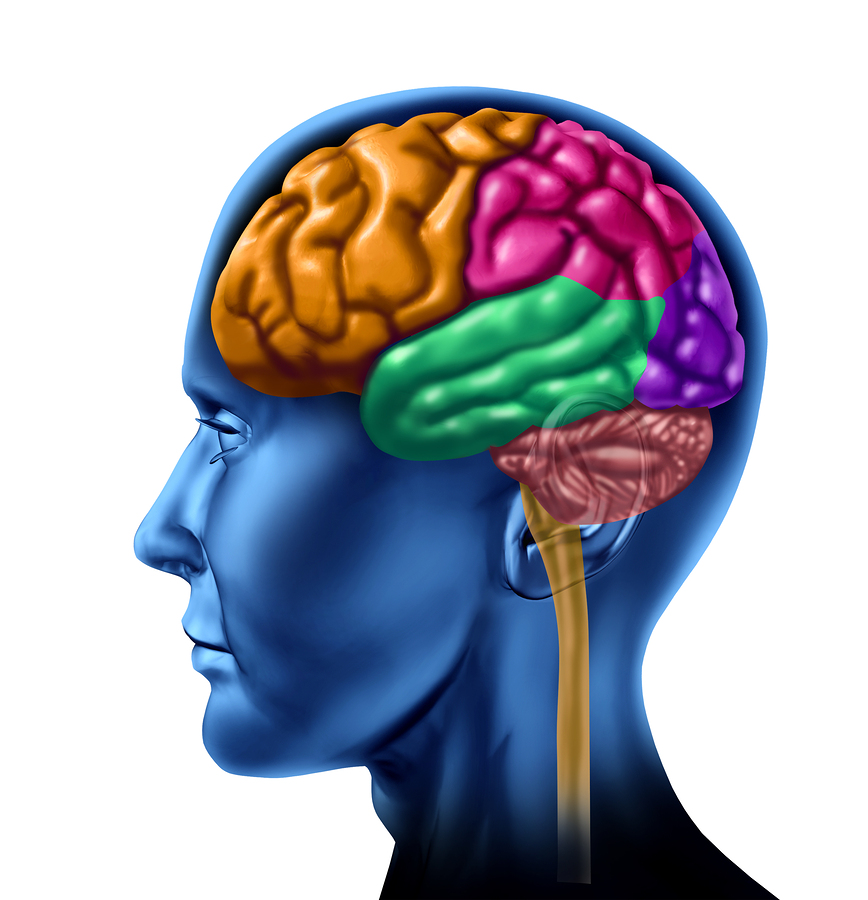
“It is a huge burden with very little actual research going into it. And still a lot of unmet medical need,” said Gabriel Baertschi, CEO of Grünenthal, a German pharmaceutical company. “The odds of succeeding in pain research are lower than in other areas. It’s much more complex than other diseases in a sense that if you hit one target you are not necessarily resolving pain. Pain is multi-dimensional. That explains why from a research point of view you don’t always succeed.”
Grünenthal is a research-oriented company that focuses on finding new treatments for conditions such as bladder pain and Complex Regional Pain Syndrome (CRPS). Recently the FDA designated an experimental drug being developed by Grünenthal as a potential breakthrough therapy for CRPS. The company is now in advanced stages of clinical trials.
Because it’s smaller and privately owned, Baertschi says Grünenthal can afford to explore new treatments for rare diseases that “Big Pharma” companies are not interested in developing.
“Most of the companies that were active in pain have closed their pain research centers,” he told PNN in an interview last month. “I think a lot of companies are pulling out because the cost of developing pain drugs has been immense. If you look at the latest generation of pain drugs, it has cost billions of dollars.
“That has scared off companies and I think companies are more focused on areas where the returns are better from a pricing point of view. Because quite frankly, if you look at oncology you can get (drug) prices that are far better than for pain.”
Insurers Refuse to Pay for New Treatments
Another problem is insurance coverage. A few years ago the U.S. Food and Drug Administration pressured drug makers to develop abuse deterrent technology for opioids to reduce the risk of abuse and addiction. Some companies spent hundreds of millions of dollars developing abuse deterrent opioids that insurers now refuse to pay for because they are more expensive.
“Payers are a huge barrier to innovative therapies because they block coverage. Without insurance coverage there is little incentive to invest,” said Lynn Webster, MD, a leading expert and researcher in pain management, who is vice president of Scientific Affairs at PRA Health Sciences.
“In the past 30 years there haven't been more than 3 new chemical entities approved by the FDA. One reason is that we don't understand enough about the different mechanisms generating pain,” Webster explained. “I see our current approach is similar to how cancer research was conducted 60 years ago. Back then most cancers were treated with the same monotherapies. Once research delved into the multi-mechanistic contributions to cancer, therapeutic advances were possible. We need to do the same for pain. And insurance has to pay for the innovations.”
“Pain is unfortunately penalized by society. People feel there is enough treatment available,” said Grünenthal’s Baertschi. “There are a lot of very good pain therapies out there. But there are quite a few areas, especially niche areas and specific pain types, that are not being treated adequately and that’s where we focus our research.”
One analyst said it is unlikely Congress will go along with the proposed cuts in the NIH budget because it funds politically popular programs.
"At worst, we believe NIH (funding) will remain flat in a continuing resolution if there is a government spending standoff," wrote Cowen analyst Doug Schenkel in a note to investors. "Although NIH funding hasn't kept up with inflation, the only time there were cuts to the agency in the past decade was when Congress' hand was forced by sequestration."
A Coalition to Save NIH Funding has also been formed to lobby against the budget cuts.
"We were dismayed to learn that the NIH is vulnerable to deep funding cuts," said Carrie Jones of JPA Health Communications, which is managing the coalition. "Each day America benefits from the innovation and scientific discoveries made at the NIH. We won't sit idly by and watch critical research be stifled."