It’s All In Your Head: How Brain Circuitry Causes Placebo Effect
/By Crystal Lindell
The placebo effect is very real. But how and why it happens has mostly remained a mystery.
However, new research may shed light on what exactly is happening in our brains when just the expectation of pain relief is sufficient for people to feel better, even when the pill or treatment they’re taking has no therapeutic value.
The discovery may even lead to new treatment options.
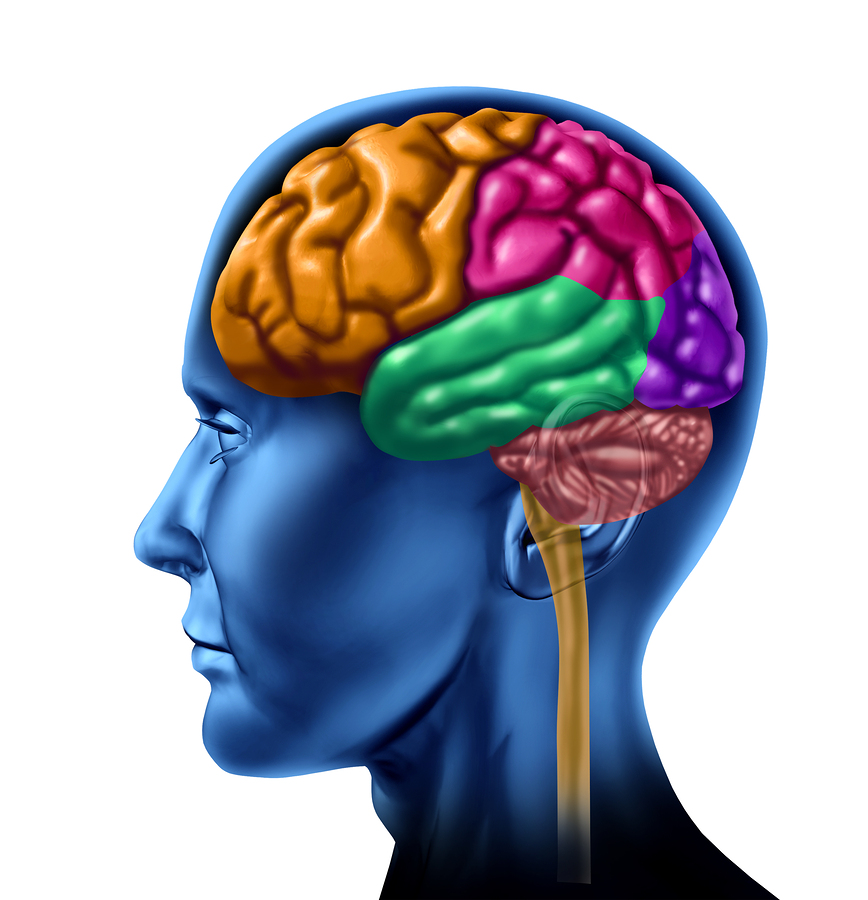
In studies on laboratory mice, researchers at the University of North Carolina School of Medicine discovered a pain control pathway that links the front of the brain, through the middle region of the brainstem, to the cerebellum in the back of the brain.
They then showed that certain parts of this pathway are activided in mice when they anticipate pain relief.
“Our results do open the possibility of activating this pathway through other therapeutic means, such as drugs or neurostimulation methods to treat pain,” says lead researcher Greg Scherrer, PharmD, associate professor in the UNC Department of Cell Biology and Physiology, who conducted the study along with colleagues at Stanford, the Howard Hughes Medical Institute, and the Allen Institute for Brain Science.
The research, recently published in the journal Nature, provides a new framework for investigating the brain pathways underlying other mind-body interactions beyond the ones involved in pain.
“We all know we need better ways to treat chronic pain, particularly treatments without harmful side effects and addictive properties,” Scherrer said. “We think our findings open the door to targeting this novel neural pain pathway to treat people in a different but potentially more effective way.”
How Scientists Studied Placebo Effect
The placebo effect is basically the brain’s way of trying to help us feel better. As such, just the expectation of pain relief is often enough to make our brains release hormones and natural chemicals that provide relief. Positive thinking and even prayer have been shown to provide similar benefits to patients, without the use of medication.
The scientific community’s understanding of the placebo effect primarily came from human brain imaging studies, which showed increased activity in certain brain regions. However, those studies did not have enough precision to show what was actually happening in those brain regions.
So Scherrer’s team designed a set of complex experiments to learn in more detail what was happening in the brain.
First, they created a method to generate in mice the expectation of pain relief. Then they used a series of experiments to study the anterior cingulate cortex (ACC) of their brains, which had previously been associated with the placebo effect.
The experiments helped them see the intricate neurobiology of the placebo effect on the receptors, neurons, and synapses of the brain. When mice expected pain relief, it boosted signaling along the pain pathway.
“There is an extraordinary abundance of opioid receptors here, supporting a role in pain modulation,” Scherrer said. “When we inhibited activity in this pathway, we realized we were disrupting placebo analgesia and decreasing pain thresholds. And then, in the absence of placebo conditioning, when we activated this pathway, we caused pain relief.”
In a 2021 study, researchers had a similar breakthrough when studying the placebo effect. Researchers at Dartmouth University conducted an analysis of neuroimaging studies involving over 600 healthy people who participated in placebo studies. Their findings showed that placebo treatments reduced pain-related activity in multiple areas of the human brain.