My Life Is on the Line Due to Rx Opioid Shortages
/By Christine Kucera, Guest Columnist
On May 24, I had my regularly scheduled pain management appointment. The prescription for my normal regimen of 10mg oxycodone was sent electronically to my local CVS pharmacy. About an hour later, I received a text from CVS saying they received the prescription from my doctor.
I followed up later through their automated system. That is the moment of shocking revelation when I learned that my prescription was not going to be filled on time, and that it may not be ready until a week after my fill date.
Utterly panicked, heart racing, thinking and speaking a mile a minute, I contacted the pharmacy. They confirmed they were out of 10mg oxycodone tablets.
“What am I supposed to do?” I asked. A woman who I don’t know replied that I should try contacting other pharmacies.
Really? I can’t do that. Pharmacies won’t tell me, the patient, if they have a supply of a controlled substance. So she looked it up and said it looks like “X” pharmacy has it and that I should have my doctor send the prescription there. Unfortunately, by the time my provider received the message, it was too late.
I made multiple calls to another pharmacy and they were extremely rude. I called my pharmacy again. This time I spoke with a pharmacist that knew me. He was very understanding, as we discussed what to do next.
CHRISTINE KUCERA
We came up with a plan. He said to have my doctor send him a prescription for 5mg oxycodone. I immediately emailed my provider about the shortage and asked him to send a new prescription for 5mg, since they were out of 10mg tablets.
It was a very long night and I was extremely anxious waiting for a reply from my provider. As a long-term opioid patient of 30 years with intractable pain, I’ve been through the unimaginable, especially after the CDC published its first opioid guideline. Since 2016, I’ve been force tapered to suboptimal treatment levels, denied pain medication during multiple hospitalizations, and told to take Tylenol.
A surgeon even used prescription fentanyl on me during an interventional procedure after being told it doesn’t work on me – leaving me awake and screaming during the procedure. That’s just to name a few examples. Believe me, there are many more.
My thoughts are racing out of control. I can’t do this anymore. I can’t live life with unrelenting, unmanaged pain all day, every day. I’m barely holding on now, trying hard not give up hope. It’s not easy living in a body that’s under assault from an invisible invader, leaving my entire body riddled with rare diseases, along with severe bone, nerve, connective tissue and organ pain.
As a person with severe medically induced PTSD, I can fully recall all of the previous times I was forced off my managed regime of opiate medication. This time it’s going to be at the hands of the DEA, which has intentionally created shortages of oxycodone.
Next day arrives, a new prescription for 5mg is sent and I sigh with relief. It was short lived. Another pharmacist said my insurance company won’t cover the 5mg substitute without prior authorization. Completely losing control of my emotions, I asked why do I need another prior authorization? My daily limit of 90 morphine milligram equivalents (MME) didn’t change, just the dose of the tablets
“It’s because of daily quantity limits,” the pharmacist replied.
Are you freaking serious? I’m out of oxycodone as of today and you’re saying I can’t have 2 weeks of a substitute because there is no supply anywhere of 10mg and my insurance has quantity limits on 5mg doses? I was angry and upset. This is so wrong! What am I supposed to do?
To that, the pharmacist says, “You can pay out of pocket.”
I didn’t have a choice, although I knew what happens from paying out of pocket with cash and sending prescriptions to new pharmacies. Those are red flags for prescription drug monitoring programs (PDMPs).
What’s next CDC and DEA? You’ve fabricated the great Opioid Lie and created policies that affect all pain care in all settings. Created new burdens for disabled and chronically ill patients. Created an opioid guideline that doesn’t allow for individualized treatment and places limits on prescriptions. You’ve shackled doctors with no options but to provide inadequate pain care or abandon patients altogether.
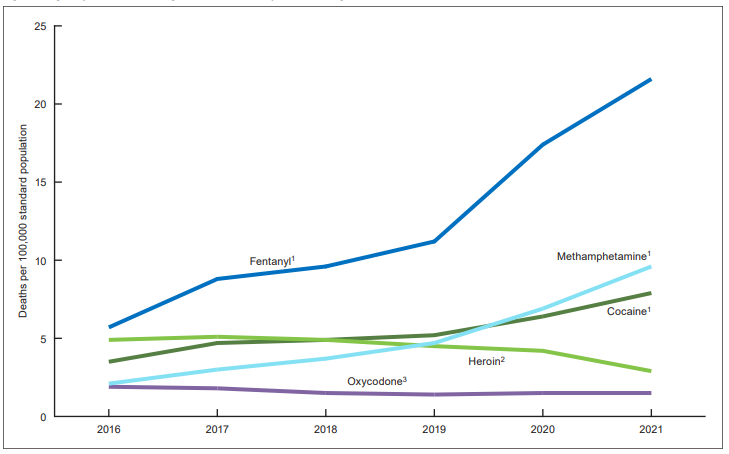
Now patients and their providers are having to deal with DEA created shortages of essential medicines. This has got to stop! Pain patients have never been the driver behind the overdose crisis. Anti-opioid prohibition policies are harming, torturing and killing U.S. citizens.
What do I do? There are no protections or even a set of procedures in place to assist patients and providers when there are shortages of controlled substances. It really is a nightmare situation. I feel helpless. The shortage is not my fault, the restrictions have gone too far, and my life is on the line.
Christine Kucera lives with psoriatic arthritis, spondyloarthropy, spondylitis, polyarthritis, sacroiliitis, degenerative joint disease, dermatomyositis, mixed connective tissue disease, spinal radiculopathy, hypoparathyroidism, rare endocrine tumors, psoriasis, endometriosis stage IV, pelvic adhesive disease, and other painful conditions.
Prior to becoming disabled, Christine was a healthcare research systems developer and analyst for federally funded CMS, AHRQ, and NIH grants and programs.
Do you have a “My Story” to share? Pain News Network invites other readers to share their stories about living with pain and treating it. We are particularly interested in your experiences dealing with current drug shortages. Send your stories to editor@painnewsnetwork.org.