What Do You Think About Changes to CDC Opioid Guideline?
/By Pat Anson, PNN Editor
Do you think the proposed changes to the CDC’s opioid guideline are an improvement over the original 2016 guideline? Will the changes make doctors more or less willing to prescribe opioids? Should the guideline be expanded to include recommendations for treating conditions like migraine and low back pain?
Those are some of the questions we’re asking in a new PNN survey on the long-awaited draft revision of the guideline that was unveiled last month by the CDC. In addition to giving healthcare providers more flexibility in using opioid medication to manage chronic pain, some experts say the changes effectively transform the guideline into a national “standard of care” for pain management – one that would apply to most doctors and patients, regardless of the severity or duration of their pain.
While the guideline changes have been applauded by professional societies like the American Medical Association for removing “arbitrary doses thresholds” for opioids, some worry that the expansion goes too far and could harm patients -- like the original guideline did -- by depriving them of effective pain treatments.
“The CDC is outside its lane to be recommending how physicians should practice pain medicine. Would they recommend how to treat hypertension or diabetes? If they did, it too would be inappropriate, unless it was in collaboration with one or more of the medical professional societies devoted to those areas,” says Lynn Webster, MD, Senior Fellow at the Center for U.S. Policy and past president of the American Academy of Pain Medicine.
“I have a lot of concerns about the new version. It is better, but still terribly misleading and not grounded in science, which is terrible disappointing.”
90 MME Threshold Dropped
Perhaps the biggest change to the 2016 guideline is the CDC’s decision to drop a recommendation that opioid doses not exceed 90 morphine milligram equivalents (MME) per day, which quickly became a hard limit for many providers, insurers, states and regulators.
While the CDC still recommends caution about doses exceeding 50 MME, that advice is not enough for Lewis Nelson, MD, a longtime critic of opioid prescribing who advised the agency when the original guideline was created. He thinks the 90 MME limit is based on sound evidence.
“There are good data to support that there is an inflection point at 90 MME. It’s clear that high-dose chronic opioid therapy is associated with a number of adverse consequences -- including addiction, unintentional overdose and potentially death,” says Nelson, the Chair of Emergency Medicine at Rutgers New Jersey Medical School. “In a way, it’s a race to the bottom in pain management, because if you’re not getting better with a reasonable dose of an opioid, there’s nothing to support that additional opioid is going to carry significant benefit and is known to markedly increase the risk.”
Dr. Webster says the use of MME to guide prescribing is misleading because not all opioids are the same or convert well to MME doses. Like others, he worries that 50 MME will become the new hard threshold for opioid doses.
“I think any reference to conversion tables and MME will be interpreted as validation of them. We saw that with the 2016 guideline,” Webster told PNN. “The CDC needs to explicitly state the lack of scientific basis for both and that their use could be dangerous in some cases. They should not cite 50 MME threshold anywhere, as it is meaningless, misleading and will lead to further misapplication of the recommendation. You would think that they would have learned that by the 2016 guideline.”
Take Our Survey
This is the fifth survey PNN has conducted on the CDC guideline. All of them found that the vast majority of patients and providers believe the guideline was harmful, worsened the quality of pain care, and led some patients to contemplate suicide or turn to street drugs.
For those who think surveys are a waste of time and the CDC doesn’t pay attention to them -- think again. On Page 53 of its revised opioid guideline, the agency cites PNN’s 2017 survey and has a footnote linking to it:
"An online (non-peer reviewed) survey of over 3000 patients 1 year after the release of the 2016 CDC Guideline found that 84% reported more pain and worse quality of life and 42% said they had considered suicide; however, the survey did not attempt to sample patients with chronic pain using a rigorous methodological approach.”
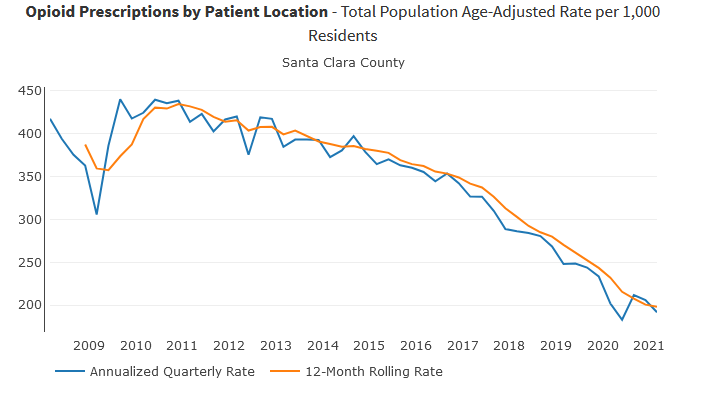
It’s true the PNN survey was not peer-reviewed and that patients were not sampled with a “rigorous methodological approach.” It’s also true that CDC has not conducted a large survey of its own to measure the impact of its guideline on patients. The agency has focused on counting opioid prescriptions — not patient outcomes — as a measure of whether its guideline is working.
To take our new survey, click here.
It should only take a few minutes to complete. We’ll share the results in mid-April.
'This is an opportunity for patients, caregivers, clinicians and others to share their impressions of the 2022 revised and expanded CDC practice guidelines for treatment of acute and chronic pain,” says patient advocate Richard “Red” Lawhern, PhD.
“This guideline will ultimately steer pain care for the foreseeable future, for better or worse. The more involved and informed every part of our community is, the more we can help shape its impact. This survey is one more way to get involved and help guide future efforts,” said Tamera Lynn Stewart, Policy Director for P3 Political Action Alliance.
You can read the revised draft of the CDC guideline and leave an online comment in the Federal Register by clicking here. Comments must be received by April 11.