Pain Is Not a Competition
/By Mia Maysack, PNN Columnist
A question I've often encountered is, “Why make pain political?”
Here's a newsflash for everyone: It was created that way. And not initially by us, I might add.
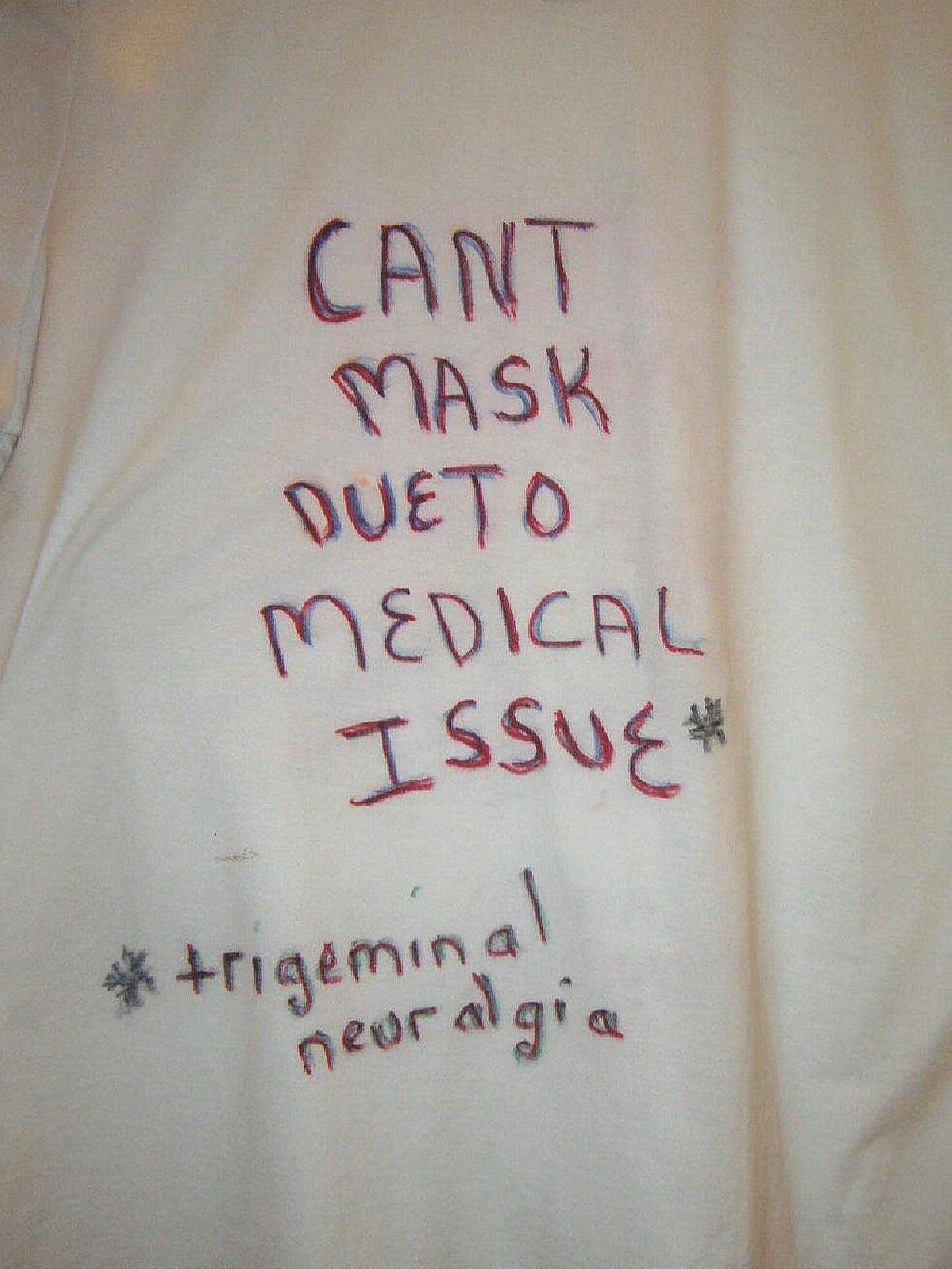
Despite having lived with chronic head pain every single day for over 20 years, I’m still fighting for a proper diagnosis. The more tests, appointments, examinations and permission slips I get only feeds into the perpetual cycle of phone tag, hold music and Zoom links. Not to mention pandemic induced anxiety.
It's all done in the name of “patient centeredness,” but I find it all confining and traumatizing.
This has led to me visiting with healthcare providers very minimally. I’m grateful to be able to slowly but surely distance myself, but I’m also aware that many won’t ever have that option or luxury. I have always been conscious of my privilege, almost dying while minding my own business as a 10-year old has a tendency to humble a person. That’s part of what fuels my fire to fight not only my own battles, but for the sake of others in the form of activism.
Common misconceptions are that a person must be able-bodied in order to participate in their own advocacy or that we are permitted only to advocate for a specific cause, such as limiting ourselves to whatever pain condition or treatment we identify with.
But if we expect people to care about what we’re going through, wouldn’t inclusiveness for other causes be a demonstration of mutual respect and support? That is lacking in the pain community and beyond.
For example, I’m severely allergic to most medications, specifically the “good stuff” for pain relief. But that hasn’t stopped me from being involved in efforts pertaining to the opioid crisis and healthcare access in general.
I was once invited to speak at a patient protest where I would have otherwise remained silent. Other patients who were there understandably did not want to be judged, ridiculed, exiled or singled out for speaking up about opioid medication, so I stepped up and shared my own story. For that, I was shamed afterwards, due to the fact I am not physically tolerant of pills!
If that ain’t political, I don’t know what is.
It has been my experience that there’s tremendous difficulty in acknowledging someone else’s perception as being equally real and valuable as one’s own. This leads to a self-defense mechanism, cultivating a sense of validation that can come across as belittling what others have gone through. No one really knows what it is like to live a day in someone else's shoes
I don’t participate in groups fixated on ONE type of ailment. Discomfort of all kinds should be invited and welcomed because hurt does not discriminate and misery can’t be measured. Pain is not a competition.
I have felt the need to step away from people who are not supportive. Instead of working to strengthen the inner bond that unites us, many would rather convey how much worse they have it than everybody else, instead of listening and learning from others.
We're in the thick of it as a collective right now. It is necessary for the sake of our lives to inch closer toward a willingness to grow and project hope, especially when it feels like there is none. That's how we can save ourselves and one another.
Focusing on what separates us as opposed to how we're able to relate as humans is overly prevalent throughout the pain community and beyond. Suffering is playing out on a global scale and is much bigger than any of us. We’ll never drive true change in healthcare if we dismantle each other instead of the systems we’re fighting against.
Mia Maysack lives with chronic migraine, cluster headache and fibromyalgia. Mia is the founder of Keepin’ Our Heads Up, a Facebook advocacy and support group, and Peace & Love, a wellness and life coaching practice for the chronically ill.