4 Tips to Avoid Chronic Pain’s Anxiety Trap
/By Jennifer Martin, PsyD, Columnist
Am I ever going to get better? Am I going to get worse?
What is in store for me next?
Is there anything I can do to make the pain go away?
How am I going to deal with this for the rest of my life?
How am I going to take care of my family?
Am I ever going to be able to be physically active again?
Am I going to be able to work or finish school?
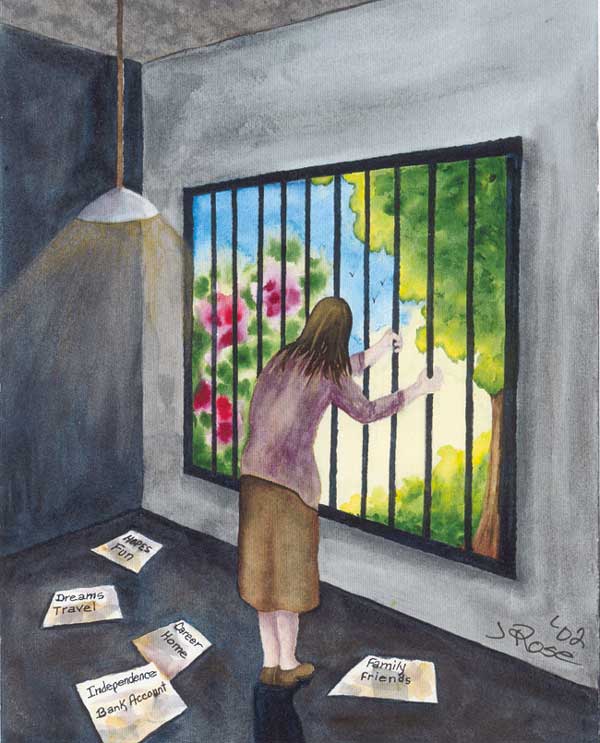
These are just some of the questions that run through the minds of those with chronic pain. For a lot of us, racing thoughts and anxiety are an unwelcome companion. The fear and anxiety come at the most inopportune times and they envelope us. Just when we think we have put the negative thoughts out of our mind, here they come again, like a wave crashing down and trapping us.
It is so important to take control of anxiety when you have chronic pain because anxiety can actually increase pain. It is a vicious cycle that can spin out of control if not treated.
Anxiety often times leads to poor sleep -- and poor sleep often leads to more pain the following day.
Anxiety also leads to negative thoughts – and negative thoughts may lead to feelings of depression, isolation, and hopelessness.
These feelings can lead to noncompliance in treatment or inactivity, which may increase pain. Anxiety can cause muscle tension and an inability to relax, which also has the ability to increase pain.
Do you see where I am going with this? Anxiety and pain are closely related.
So, if you are suffering from anxiety and a chronic condition, what can you do? Here are four tips to avoid or diminish anxiety:
1) Distract yourself as much as you can: When you begin to notice anxious thoughts, tell yourself “STOP” and then focus your attention on something you enjoy. Whether it is relaxing thoughts of the beach or an activity such as painting, talking with a friend, or watching TV, distraction will get your attention away from your anxious thoughts and onto something else.
2) Exercise: Exercise does not have to be physically strenuous. Take a 10 or 15-minute walk while listening to an iPod or book on tape. Stretch for fifteen minutes. Research some gentle yoga poses. Anything you can find that works for you that does not increase your pain is great. Exercise can do amazing things for your state of mind and those tense, anxious muscles.
3) Find help and support: Support groups are wonderful places. I always tell people, “You cannot really understand what it is like to have chronic pain or a chronic illness unless you have one.”
Having a chronic condition can feel extremely lonely, even in the most crowded places. Support groups offer a non-judgmental atmosphere filled with people who have some understanding of what you are going through.
Individual therapy is also a great option, particularly if you don’t want to talk about what you are going through with friends, family or in a group of people. It is a great place to learn additional tools and coping techniques to help deal with chronic pain and anxiety.
4) Breathe: Research different breathing techniques. Learning to slow your breathing when you are experiencing anxiety will not only calm your mind, it will calm your body too, thus helping your pain.
If you have chronic pain and anxiety, start today and help yourself get help. Even if it only helps your pain a little bit, isn’t it worth it?
Jennifer Martin, PsyD, is a licensed psychologist in Newport Beach, California who suffers from rheumatoid arthritis and ulcerative colitis. In her blog “Your Color Looks Good” Jennifer writes about the psychological aspects of dealing with chronic pain and illness.
Jennifer is a professional member of the Crohn’s and Colitis Foundation of America and has a Facebook page dedicated to providing support and information to people with Crohn’s, colitis and other digestive diseases.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.