Study: Some Brains ‘Hardwired’ for Chronic Pain
/By Pat Anson, Editor
Why do some people develop chronic pain from an injury or illness, while others do not?
The answer to that question may really be all in our heads.
A groundbreaking study by scientists at Northwestern University and the Rehabilitation Institute of Chicago (RIC) found that some people are genetically predisposed to chronic pain because of brain “abnormalities” that raise their risk of developing chronic pain. The findings challenge long-standing views on the science of pain, which emphasize treating pain at the site of the initial injury.
"While simple, the logic of addressing problems at the site of an injury to remove pain has resulted in only limited success," said senior study author Marwan Baliki, PhD, a research scientist at RIC and an assistant professor of physical medicine and rehabilitation at Northwestern University Feinberg School of Medicine.
"The central processes of chronic pain have largely been ignored, so our research team set out to better understand the brain's role."
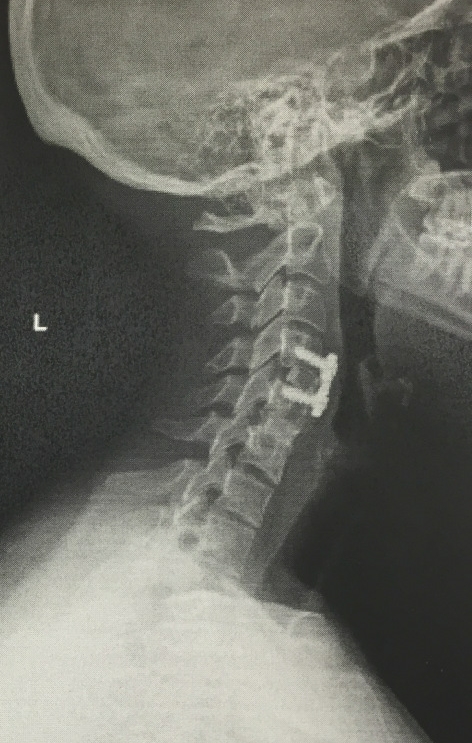
Baliki and his colleagues conducted the first longitudinal brain imaging study, which tracked 159 patients for three years following an acute back injury, along with 29 healthy control subjects.
MRI brain scans were conducted on all of the participants five times during the course of the study.
The researchers found that patients who developed chronic pain from their back injury had a smaller hippocampus and amygdala compared to those who recovered from the injury and the healthy control subjects.
The hippocampus is the primary brain region involved in memory formation and retention, while the amygdala is involved in the processing of emotions and fear. In addition to size variations, these brain regions also showed differences in connections to the rest of the brain, particularly to the frontal cortex, an area involved in judgment.
Together, the researchers estimate that these brain differences accounted for about 60% of the chronic pain felt by participants.
Most importantly, the study also revealed that the volumes of the amygdala and hippocampus did not change over the course of the study, suggesting that those who developed chronic pain were genetically predisposed to it.
"Here we establish that the gross anatomical properties of the corticolimbic brain, not the initial back pain, determine most of the risk for developing chronic pain," said first author Etienne Vachon-Presseau, PhD, a visiting postdoctoral fellow in physiology at Feinberg.
“As the anatomical risk factors were stable across 3 years, they were presumably hardwired and present prior to the event initiating back pain. These results pave the way for the development of novel and distinct approaches to prevention and treatment of chronic pain.”
The Northwestern and RIC study will be published in the June edition of the journal Brain.