Ironic Partners: Suicide Prevention and Pain Awareness Month
/By Dr. Lynn Webster, PNN Columnist
September is National Suicide Prevention Month. It is also Pain Awareness Month. It may appear coincidental or ironic that we recognize suicide and pain during the same month. However, there is an unfortunate association between the two: pain -- either emotional or physical -- too often leads to suicide. Conversely, awareness and treatment of either type of pain, can often prevent suicide.
According to the World Health Organization, 800,000 people worldwide take their own lives each year. The number of suicide attempts is many times greater. Suicide is a serious problem globally and it is often linked to mental health problems.
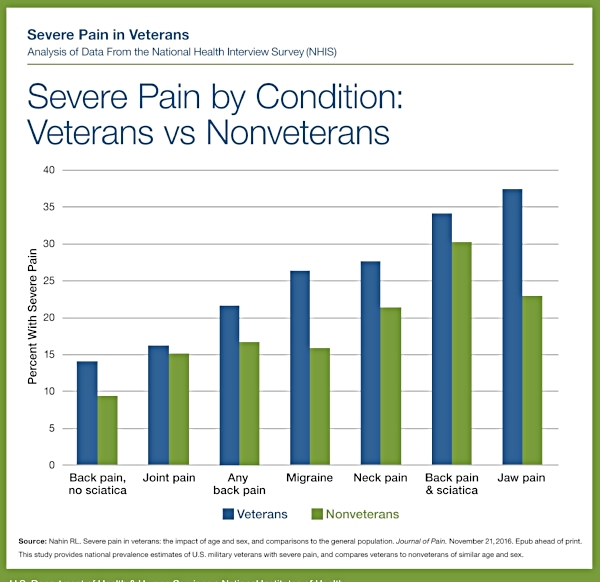
Many military veterans, like civilians, suffer from both physical and emotional pain. This can lead to substance abuse and increased suicide risk. Veterans frequently experience post-traumatic stress disorder (PTSD) as a result of their military service, but they often don’t get the help they need because the military's mental health system may not take their struggles seriously. The Pentagon has even refused to award Purple Hearts to veterans with PTSD because it is not considered a physical wound.
Transitioning to civilian life after leaving the military can be stressful due to disruptions in social support, financial strain and changes in access to health care. Between 6 and 12 months after they separate from the military, veterans are at the highest risk of suicide.
Suicides associated with serving in the military are at a crisis level -- perhaps because of a lack of pain awareness and cuts in funding to suicide prevention programs. The Department of Veterans Affairs estimates 17 veterans commit suicide every day. Veterans' suicides account for 18% of all suicides in the U.S., even though veterans only make up 8.5 percent of the adult population.
More People at Risk
It’s not just veterans at risk. Over 48,000 Americans took their own lives in 2018. The suicide rate in the U.S. has increased by about 1.8% annually since the year 2000 and is one of the highest among wealthy nations.
The coronavirus pandemic may be adding to the problem. According to the Centers for Disease Control and Prevention, adults have recently reported considerably increased adverse mental health conditions associated with COVID-19. The CDC says groups that are suffering the greatest numbers of COVID-19 cases, including minorities, essential workers and caregivers, have experienced “disproportionately worse mental health outcomes, increased substance use, and elevated suicidal ideation."
People with substance use disorders are also more likely to contract the coronavirus. Those who do become infected bear the double burden of COVID-19 and addiction.
All suicides are tragic, and the losses affect families and entire communities. But suicides can be prevented by understanding the warning signs. Aggression, mood changes, relationship problems, prolonged stress, another person's suicide, and access to firearms or lethal drugs are all risk factors. Intractable pain, too, is a red flag.
According to the American Foundation for Suicide Prevention, depression, substance use disorders, bipolar disorder, and schizophrenia all elevate the possibility of suicide.
Suicidality has become omnipresent in our society. We probably all know of someone who has committed suicide. Even worse, we may have lost a family member or loved one due to suicide. It affects people of all socio-economic levels.
The National Suicide Prevention Lifeline (1-800-273-8255) provides a hotline for anyone who is having a mental health crisis or suicidal thoughts. Free, confidential help for a loved one, or for you, is only a phone call — or online chat — away.
We may not always know who is struggling with emotional pain, but it is generally apparent when someone experiences insufferable physical pain. The partnership between suicide ideation and severe untreated pain can be mitigated if society will see people in pain as deserving of treatment.
Lynn R. Webster, MD, is a vice president of scientific affairs for PRA Health Sciences and consults with the pharmaceutical industry. He is author of the award-winning book The Painful Truth, and co-producer of the documentary It Hurts Until You Die. Opinions expressed here are those of the author alone and do not reflect the views or policy of PRA Health Sciences. You can find him on Twitter: @LynnRWebsterMD.