Experimental Implant Uses Coolant to Numb Nerve Pain
/By Pat Anson, PNN Editor
Applying ice on inflamed tissues and sore muscles is one of the oldest ways to relieve pain and promote healing. Researchers at Northwestern University are taking that tried-and-true method a step further, with the development of a small, flexible implant that can alleviate pain by literally cooling nerves.
Researchers believe the experimental implant could be most beneficial to patients who undergo surgeries, nerve grafts or even amputations. Surgeons could implant the device during the procedure to help patients manage post-operative pain on demand without the use of drugs.
“As engineers, we are motivated by the idea of treating pain without drugs — in ways that can be turned on and off instantly, with user control over the intensity of relief,” says John Rogers, PhD, Professor of Materials Science and Engineering at Northwestern and lead author of a study published in the journal Science.
“The technology reported here exploits mechanisms that have some similarities to those that cause your fingers to feel numb when cold. Our implant allows that effect to be produced in a programmable way, directly and locally to targeted nerves, even those deep within surrounding soft tissues.”
In experiments on laboratory rats, Rogers and his colleagues demonstrated that the implants can rapidly cool peripheral nerves to relieve neuropathic pain.
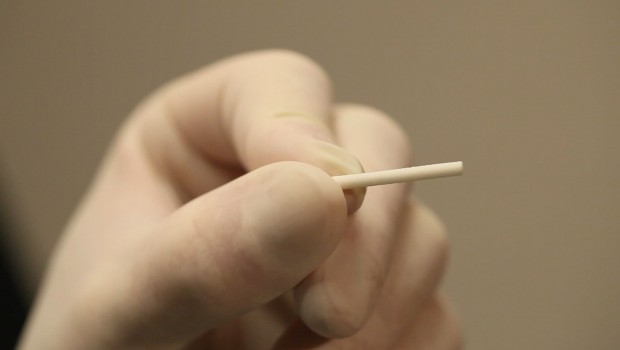
As thick as a sheet of paper, at its widest point the implant is 5 millimeters wide – about the size of the eraser on a pencil. One end is curled into a cuff that can softly wrap around a nerve, without the need for sutures to hold it in place.
“If you think about soft tissues, fragile nerves and a body that’s in constant motion, any interfacing device must have the ability to flex, bend, twist and stretch easily and naturally,” said Rogers.
NORTHWESTERN UNIVERSITY
To induce cooling, the device contains tiny microfluid channels. One channel contains a liquid coolant (perfluoropentane), while a second channel contains dry nitrogen. When the liquid and gas flow into a shared chamber, a reaction occurs that causes the liquid to evaporate and cool. A tiny sensor in the implant monitors the temperature of the nerve to ensure that it’s not getting too cold, which could cause tissue damage.
“As you cool down a nerve, the signals that travel through the nerve become slower and slower — eventually stopping completely,” said coauthor Matthew MacEwan, PhD, from Washington University School of Medicine in St. Louis. “We are specifically targeting peripheral nerves, which connect your brain and your spinal cord to the rest of your body. These are the nerves that communicate sensory stimuli, including pain. By delivering a cooling effect to just one or two targeted nerves, we can effectively modulate pain signals in one specific region of the body.”
An external pump allows patients to remotely activate the implant and increase or decrease its intensity. Because the device is biocompatible and water-soluble, it will naturally dissolve and absorb into the body over the course of days or weeks — bypassing the need for surgical extraction.
Other cooling therapies have been tested experimentally, but have limitations. Instead of targeting specific nerves, they cool large areas of tissue, potentially leading to side effects such as tissue damage and inflammation.
“You don’t want to inadvertently cool other nerves or the tissues that are unrelated to the nerve transmitting the painful stimuli,” MacEwan said. “We want to block the pain signals, not the nerves that control motor function and enables you to use your hand, for example.”