Why IQ Isn’t Enough for Pain Care
/By Pat Akerberg, Columnist
Our once patient-centric healthcare system has been upended and turned into a profit-over-people financial equation.
Consequently, patients feel their concerns are intentionally disregarded while medical practitioners are ham strung by compromised standards. I wonder if they are as disillusioned as we are with timed, cookie-cutter treatment approaches that reinforce unsettling disconnects.
One such disconnect involves an underrated, often missing link – empathy – considered one of the most effective aspects of an outstanding healthcare practitioner.
Empathy is compassion for the chronic illness, pain and impairments their patients endure.
In his 2005 groundbreaking book, “Emotional Intelligence: Why It Can Matter More Than IQ,” Daniel Goleman made the case for empathy to be recognized as an essential component for emotional intelligence.
Differing from the intellectual focus of IQ, empathy is one of the 5 essential dimensions that make up ones’ emotional quotient or emotional intelligence – “EQ” for short.
- Emotional self-awareness: Knowing what one is feeling at any given time and understanding the impact those moods have on others
- Self-regulation: Controlling or redirecting one’s emotions; anticipating consequences before acting on impulse
- Internal Motivation: Utilizing emotional factors to achieve goals, enjoy the learning process and persevere in the face of obstacles
- Empathy: Sensing and responding effectively to the emotions of others
- Social skills: Managing relationships, inspiring others and creating connections
The key point behind EQ is that it can often matter more than IQ or technical training alone. While IQ may typically get someone hired or gain them entry, the EQ factor is what gets them promoted, predicts excellence and professional success.
Possessing both IQ and EQ is considered a winning combination in any role or field. But not everyone acquires that golden pair without awareness and training -- unless they are uniquely and naturally skilled at both.
Our medical practitioners (regulators and stakeholders) are no exception to this. In fact, the widespread distortions and neglect surrounding our side of the pain care equation and story clearly demonstrate the kind of harm pervasive EQ blind spots can do.
We’ve all experienced those rare physicians and practitioners who are both competent and capable of conveying a caring approach and empathetic style. Even if medications and various treatments fall short in addressing our chronic illnesses, their support and desire to help us never falters.
It helps immeasurably to know they’re in our corner. Physical healing may not always be possible given our circumstances, but that’s not the only kind of healing that matters. The presence of such EQ far outweighs the deficits of an approach without it. Numerous studies confirm that such human consideration and concern delivers a positive placebo effect that can’t be underestimated.
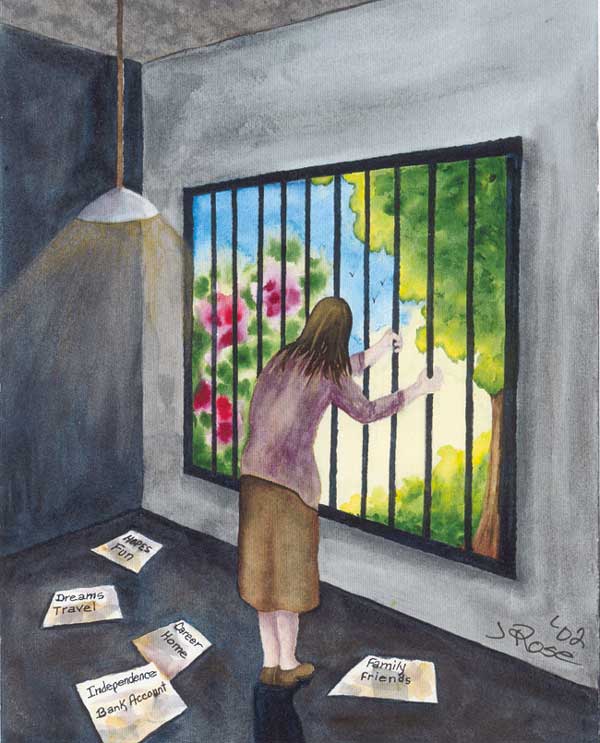
Pain patients already endure more than most will ever face. We suffer even further when our practitioners and administrators lack or devalue the human understanding EQ brings.
So how effective are our practitioners at delivering that kind of humanistic medical care in our current system?
Using the 5 factors for EQ, I did a personal rating of all of the practitioners I’ve seen since the start of my trigeminal neuralgia. It turns out that 30% on my list are high in EQ. Unfortunately, that means that 70% fall short.
The stand out characteristics that I look for made those 30% rank far above the 70% include:
- Being personable
- Making eye contact with me (not a computer screen)
- Showing true interest in my level of pain
- Patiently and intently listening to my answers
- Being open to my questions
- Offering tailored options
- Expressing empathy or gestures of concern
- Thinking outside the box for solutions
- Collaborating
- Treating me like an important partner and a helpful staff
The reasons that some practitioners or institutions may or may not possess or demonstrate empathy vary as much as our illnesses do. The good news is that once a person becomes self aware and motivated, EQ and empathy can be learned thanks to plasticity, our brains’ ability to change.
There’s no formal assessment that I know of that measures the damaging, stressful effects of chronic pain and illness when coupled with the double whammy of marginalized or impersonal healthcare.
However, like an IQ test, there is a formal assessment that determines a persons’ EQ status on all five dimensions. For a better tomorrow, there’s no reason that this assessment couldn’t be required at the start of medical training programs (doctors, nurses, physical therapists) to identify a students’ strengths and needs.
Taking it further, educational institutions can also borrow from a virtual reality learning tool developed by Embodied Labs founder Carrie Shaw, which she used to increase her understanding about her mother’s experience with dementia.
With the intention of bridging the life experience-understanding-empathy gap for young medical students, John’s Hopkins recently experimented with this technology. The project, “We Are Alfred,” gave students hands-on experience of what it’s like to be a 74- year old dealing with impairments in sight, hearing, and memory. The simulation demonstrated that you can develop EQ skills and foster understanding between practitioners and patients by giving students a slice of what their patients have to deal with.
Many times I’ve wished that the severe face pain that I experience could be simulated so that practitioners (and others) could experience what it feels like. I bet you have too.
Wouldn’t it be great, even fitting, for our government to sponsor an initiative to simulate pain? Maybe then the reality of debilitating pain would finally trump the punitive intellectual biases blocking the balanced approach EQ brings about.
Meanwhile, I’m all for efforts that aim to reinforce the message to our medical practitioners and facilities, educational institutions, government regulators, insurance companies, Big Pharma and other stakeholders that no one cares what you might know (IQ) until they know that you care (EQ).
Pat Akerberg suffers from trigeminal neuralgia, a rare facial pain disorder. Pat is a member of the TNA Facial Pain Association and is a supporter of the Trigeminal Neuralgia Research Foundation.
Pat draws from her extensive background as an organizational effectiveness consultant who coached and developed top executives, mobilized change initiatives, and directed communications.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.