I was determined to be an educated consumer in my quest to relieve pain, but time was of the essence. It’s brutal being in constant severe pain. It not only hurts, it’s exhausting. Fighting the hurt, trying to stay positive, trying to do your daily stuff, trying to be friendly, just trying to smile becomes harder and harder. .
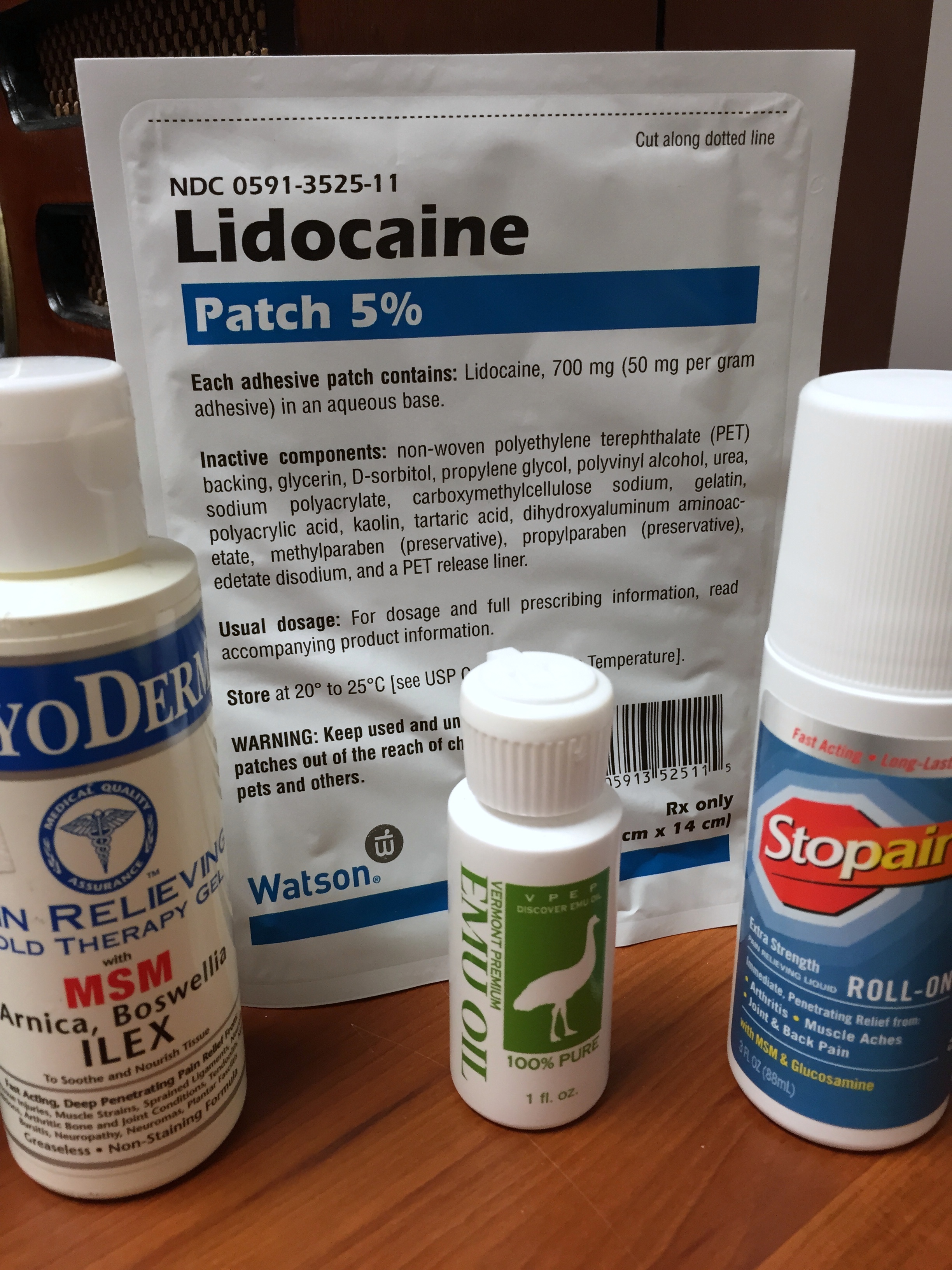
I had done enough periodic trials of opioids to know several things. They work. But then at a certain point they don’t work as well. Even upping the dosage works for only so long. I can take an opioid for breakthrough pain or an extended release opioid, but the weird haze I’d get, the strange cloudy, foggy feelings I have, I never felt normal doing them.
I mean, is that what I want to feel like for years to come? I hate the pain, but the opioid cloud from any extended use I hate also. And the risks: tolerance, dependence, respiratory distress, sexual disruption, and constipation. That last one can be a bitch. I didn’t want to live in pain. but I didn’t want the risks and that overall crap feeling that opioids presented me. So the search for alternative pain therapies was on.
Let me first say I had to have the right attitude. “Stinkin-thinkin” is out, or as my meditation expert friend says, “If you “awful-ize” regularly you will feel awful.” I cannot emphasize enough the benefit of staying upbeat. I’m not stupid, I get it. You feel horrible, you feel like crap, you want to crawl out of your skin. But I have a choice; get swallowed up in negative thoughts and that is where I’ll stay, or stay as positive as I can and that is where I’ll stay. Not easy by any means, but it is the only means for me.
I was always athletic but I smoked. Smoked from 24 years of age to 56. That had to stop. When I had my second hip replacement I said I would quit right as I entered the hospital. I did and I could write a book on that fun trip.
I knew my diet would have to change. Didn’t want anymore extra weight and I knew I needed to increase my intake of foods that reduce inflammation. I love hot peppers, love those oily fish, those greens like spinach, kale, collard greens, those whole grains, and those almonds (but gotta watch the calories).
It took hard work to stop smoking and change my diet. And there was still a whole bunch more to come. I wanted to exercise more, I wanted to do my physical therapy exercises and stretches regularly, I wanted to give basic yoga posturing a try, I wanted to do some sort of meditation/positive visualizing practice.
I had read about all the benefits these could offer and I also knew it wouldn’t come quick. THIS IS THE HARD PART. I knew I would have to stick with it. I know too many people who say they’re going to make changes in their health status and do not stick with it. They’re in abundance after all those New Year’s resolutions every January, right? I’ve been one of them any number of times! It’s much easier to stop all the hard work and a whole lot easier to just take the pills.
But not this time. I knew that if my chosen alternative pain strategies were to work, I would have to be loyal to them and I would have to give them time. A lot of time, like 3-6 months of everyday, regular time. I have a family, I was working, I had all the stuff that comes with life, and now I had to fit a bunch more things in. I had to get up earlier than before, I had to spend an hour and half to two hours at night after work doing things I hadn’t before, and I had to fit these things into my weekends as well.
My Exercise Regimen
I had a YMCA membership and it’s amazing how many free or very low cost add-ons they provide. Yoga was free. Fairly low cost trainer sessions. My insurance covered a certain amount of physical therapy. A colleague-friend at work was a meditation expert. I get a lot of free senior citizen exercise and healthy activity benefits from the town I live in.
I started an exercise regimen that included cardiopulmonary exercise, weight training, and core exercise. I do an hour and half a day, 6 days a week. The myriad PT exercises and stretches I learned had to be done every day, 7 days a week as well. I don’t do all I know every time, but I usually spend about 20 minutes to a half hour on these.
The meditation/visualization I do is a form of guided imagery. Real easy to learn and real calming to do. I conjure peaceful, beautiful images for a 15 minute period in the morning and before bed I do 15 minutes of a mindfulness type experience where I am aware of positive thoughts, feelings, and images. I try to put my pain into a corner and focus on just the other things.
The yoga may give me the most benefits. I just do poses and stretches. I incorporate most of them in my daily workout routine and at times combine them with my PT work. All nothing real fancy, or too in-depth, but just enough of the basics to really help.
I lost count how many times I would bitch and complain in the beginning. How many times did I feel all this stuff was a waste? How many times would I curse them? How many times my pain hurt when I did them? How many times was my pain worse right after them? How many times did I want to give up? How many times did I want to just take the opioids? The answers: MANY!
A month went by…two months…three months…and I started to actually feel better. My pain was being mitigated. Six months and they worked even better. And now, almost 7 years later, they work better than ever. And my opioids? I am prescribed oxycodone, but I only take it every other day or every two days. I try to allocate myself no more than 10 pills a week.
Do I still have pain? Yep. Do the opioids help? Yep. In fact, when I take them they work as effectively as the first day I started taking them. I know I could easily do more and, considering the level of pain I have, they are easily warranted. But my pain is mitigated by my alternative pain management and my opioid use is minimized.
Just as important, there has been another benefit. The cervical spine surgery that I should be eligible for I don’t have to do because my functioning is normal. You don’t do this surgery unless your functionality suffers considerably. Removing 2-3 discs, shaving down multiple osteophytes, and fusing 3-4 vertebras pose considerable post-op risks and perhaps even more pain. I’ve been told that my function is so good because of all the exercises I do, so no surgery for now.
Like I said, I can only speak for myself. But I have found a very effective balance to mitigating my pain through alternative pain management and the limited use of opioids. I still have pain every day but I manage it with a lot of hard work.
I know there are many people out there that must take opioids every day. And they should be provided with them. But I felt that I would be cheating myself if I didn’t do my best to mitigate my pain through alternative means.
I always have to be honest with myself. Am I doing all I can to ease my pain other than by taking opioid medication?