Why Does Menopause Worsen Rheumatoid Arthritis?
/By Pat Anson, Editor
A large new study is confirming what many women with rheumatoid arthritis (RA) already know – menopause and hormonal changes can significantly worsen their pain and other symptoms. But it's not clear why that happens.
Researchers at the University of Nebraska Medical Center enrolled over 8,000 women with RA – both young and old -- in their observational study. They found that post-menopausal women with RA had a significant increase in the level and rate of functional physical decline. Menopause was also associated with a worsening progression of the disease.
RA is a chronic and disabling autoimmune disease in which the body’s own defenses attack joint tissues, causing pain, inflammation and joint erosion. Women experience RA at a rate three times greater than men, have more severe symptoms and increased disability.
Previous studies have shown that women with RA experience changes in their disease during reproductive and hormonal changes. During pregnancy, women are less likely to develop RA, yet the disease is more likely to progress and flare during the post-partum period. Similarly, women who experience early menopause are more likely to develop RA compared to those who experience normal or late menopause.
Hormone levels of estrogen increase during pregnancy and decline during menopause – but the association with RA is not fully understood.
"Further study is needed as to why women with rheumatoid arthritis are suffering a greater decline in function after menopause," said the study's lead author, Elizabeth Mollard, PhD, an assistant professor in the College of Nursing at the University of Nebraska Medical Center.
"Not only is this decline causing suffering for women, it is costly to both individuals and the healthcare system as a whole. Research is specifically needed on the mechanism connecting these variables with the eventual goal of identifying interventions that can maintain or improve function in postmenopausal women with rheumatoid arthritis."
The study is published in the journal Rheumatology.
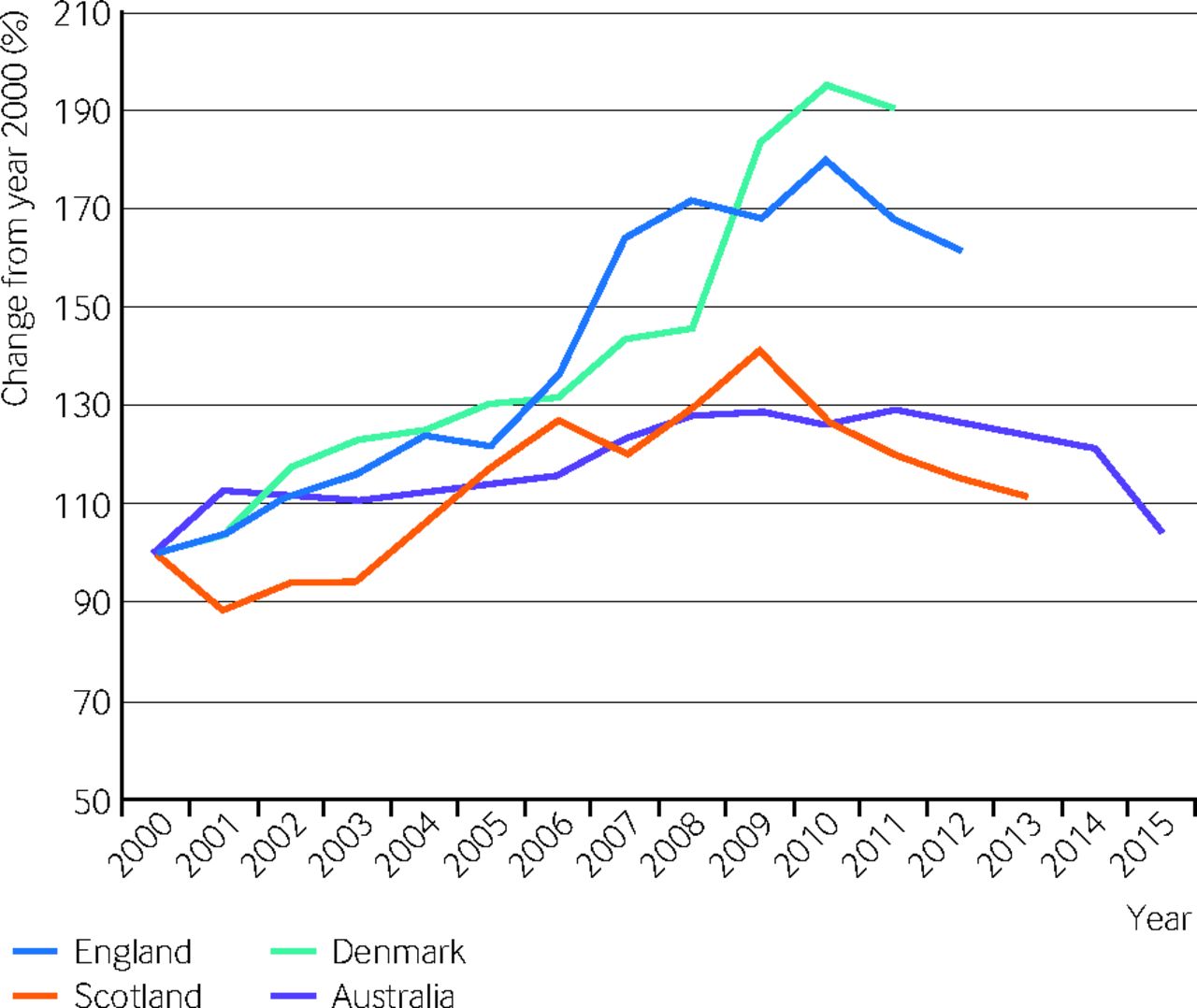
RA affects about 1.3 million Americans and about one percent of the global population. Until the late 1990s, one in three RA patients were permanently disabled within five years of disease onset.
Although there are still no cures for RA, in recent years there has been significant improvement in treatment, with disease control now possible for many patients who receive biologic drugs. Those treatments are expensive, with some biologic therapies costing $25,000 a year.