‘Amazing’ New Stem Cell Treatment for Neuropathy
/By Pat Anson, Editor
Researchers at Duke University say an experimental stem cell therapy being tested on animals shows great potential to provide long-lasting pain relief for people suffering from diabetic neuropathy or other types of nerve damage.
In a study published in the Journal of Clinical Investigation, researchers said mice injected with a type of stem cell known as bone marrow stromal cells (BMSCs) were much less sensitive to nerve pain.
"This analgesic effect was amazing," said Ru-Rong Ji, PhD, a professor of anesthesiology and neurobiology in the Duke School of Medicine. "Normally, if you give an analgesic, you see pain relief for a few hours, at most a few days. But with bone marrow stem cells, after a single injection we saw pain relief over four to five weeks."
BMSCs are known to produce an array of healing factors and can be coaxed into forming other types of cells in the body. They are already being used to treat people with serious burns, inflammatory bowel disease, heart damage and stroke.
"Based on these new results, we have the know-how and we can further engineer and improve the cells to maximize their beneficial effects," said Ji.
Researchers injected the mice with stem cells through a lumbar puncture, infusing them into the fluid that bathes the spinal cord.
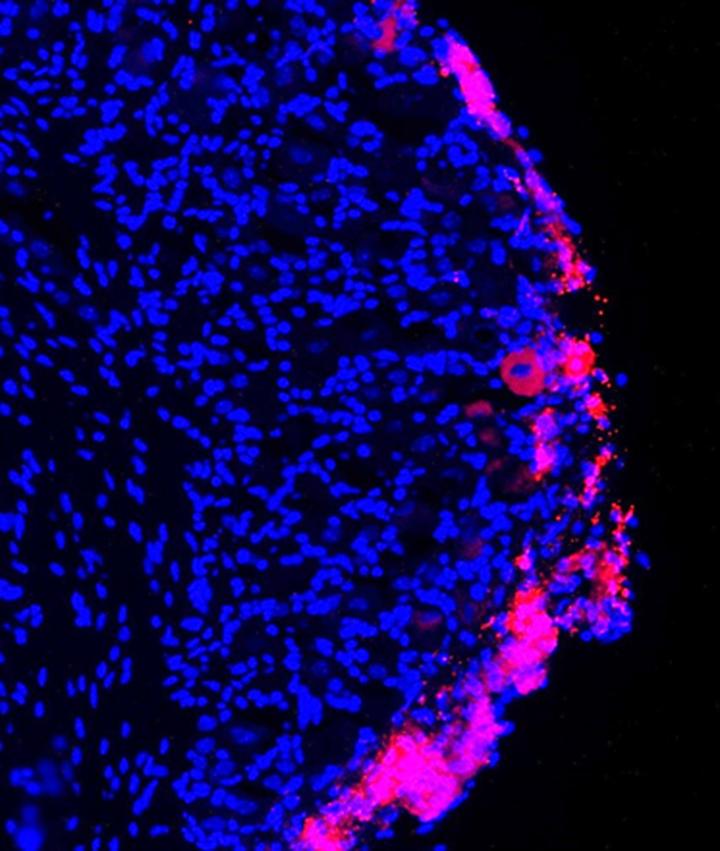
The picture on the right shows how the injected stem cells (in red) migrated to the site of the nerve injury and were still present four weeks after treatment.
A molecule emitted from the injured nerve cells -- which has previously been linked to neuropathic pain – is believed to act as a “homing signal” and attract the stem cells.
Researchers measured levels of anti-inflammatory molecules in the mice and found that one in particular, TGF-β1, was present in higher amounts in the spinal fluid of the stem cell-treated animals.
TGF-β1 is a protein that is secreted by immune cells and is common throughout the body. Research has shown that people with chronic pain have too little TGF-β1.
courtesy duke university
Injecting TGF-β1 directly into spinal cord fluid provides pain relief, but only for a few hours, according to Ji. By contrast, bone marrow stromal cells stay on site for as much as three months after the infusion.
Ji’s research team is working to identify stem cells that produce more TGF-β1, as well as other types of pain relieving molecules. In addition to diabetic neuropathy, researchers believe stem cell therapy could also be used to treat pain from chemotherapy, surgical amputation, lower back pain and spinal cord injuries.
Nearly 26 million people in the United States have diabetes and about half have some form of neuropathy, according to the American Diabetes Association. Diabetic peripheral neuropathy causes nerves to send out abnormal signals. Patients feel pain or loss of feeling in their toes, feet, legs, hands and arms. It may also include a persistent burning, tingling or prickling sensation. The condition can lead to injuries, chronic foot ulcers and even amputations.
Another recent animal study by researchers in the U.S. and South Korea found that diabetic rats given intramuscular injections of bone marrow stromal cells experienced both angiogenesis (blood vessel growth) and a restoration of the myelin sheath -- a protective covering over nerve cells damaged by neuropathy.
"Currently, the only treatment options available for DN (diabetic neuropathy) are palliative in nature, or are directed at slowing the progression of the disease by tightly controlling blood sugar levels," said Dr. John Sladek, Jr., Professor of Neurology, Pediatrics, and Neuroscience, Department of Neurology at the University of Colorado School of Medicine.
"This study offers new insight into the benefits of cell therapy as a possible treatment option for a disease that significantly diminishes quality of life for diabetic patients.”
The study is being published in the journal Cell Transplantation.