Patients With Epilepsy Navigate Murky CBD Market
/By Eric Berger, Kaiser Health News
In 2013, Tonya Taylor was suicidal because her epileptic seizures persisted despite taking a long list of medications.
Then a fellow patient at a Denver neurologist’s office mentioned something that gave Taylor hope: a CBD oil called Charlotte’s Web. The person told her the oil helped people with uncontrolled epilepsy. However, the doctor would discuss it only “off the record” because CBD was illegal under federal law, and he worried about his hospital losing funding, Taylor said.
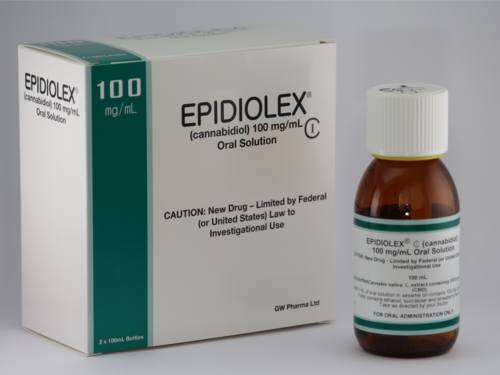
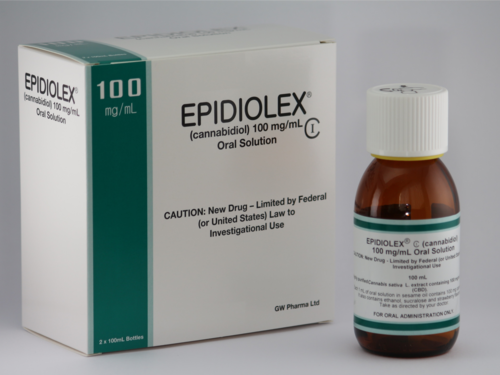
The federal government has since legalized CBD, and it has become a multibillion-dollar industry. The FDA also has approved one cannabis-derived prescription drug, Epidiolex, for three rare seizure disorders.
But not much has changed for people with other forms of epilepsy like Taylor who want advice from their doctors about CBD. Dr. Joseph Sirven, a Florida neurologist who specializes in epilepsy, said all of his patients now ask about it. Despite the buzz around it, he and other physicians say they are reluctant to advise patients on over-the-counter CBD because they don’t know what’s in the bottles.
The FDA does little to regulate CBD, so trade groups admit that the marketplace includes potentially harmful products and that quality varies widely. They say pending bipartisan federal legislation would protect those who use CBD. But some consumer advocacy groups say the bills would have the opposite effect.
Caught in the middle are Taylor and other patients desperate to stop losing consciousness and having convulsions, among other symptoms of epilepsy. They must navigate the sometimes-murky CBD market without the benefit of regulations, guidance from doctors, or coverage from health insurers. In short, they are “at the mercy and the trust of the grower,” said Sirven, who practices at the Mayo Clinic in Jacksonville.
While the CBD industry is new territory for the FDA, people have used cannabis to treat epilepsy for centuries, according to a report co-authored by Sirven in the journal Epilepsy & Behavior.
More than 180 years ago, an Irish physician administered drops from a hemp tincture to an infant experiencing severe convulsions. “The child is now in the enjoyment of robust health, and has regained her natural plump and happy appearance,” Dr. William Brooke O’Shaughnessy wrote at the time.
Charlotte’s Web
Much of the recent interest in CBD stemmed from the 2013 CNN documentary “Weed,” which featured Charlotte Figi, then 5, who had hundreds of seizures each week. With the use of CBD oil, her seizures suddenly stopped, CNN reported. After that, hundreds of families with children like Charlotte migrated to Colorado, which had legalized marijuana in 2012.
Then in 2018, the federal government removed hemp from the controlled substances list, which allowed companies to ship CBD across state lines and meant families no longer needed to relocate.
The FDA still prohibits companies from marketing CBD products as dietary supplements and making claims about their benefits for conditions such as epilepsy.
“The FDA has really done little to protect consumers from an unregulated marketplace that they have created.”
The agency is gathering “research, data and other safety and public health input to inform our approach and to address consumer access in a way that protects public health and maintains incentives for cannabis drug development through established regulatory pathways,” Dr. Janet Woodcock, then the FDA’s acting commissioner, said in 2021, according to a dietary supplements trade group.
“The FDA has really done little to protect consumers from an unregulated marketplace that they have created,” said Megan Olsen, general counsel for the Council for Responsible Nutrition, a different dietary supplements trade group.
A recent study in Epilepsy & Behavior on 11 oils found that three contained less CBD than claimed, while four contained more. Charlotte’s Web contained 28% more CBD than advertised, according to the report. The study also pointed out that the problems “mirror concerns” raised for generic anti-seizure medications, which the FDA does regulate.
“I’m not anti-CBD,” said Barry Gidal, a professor of pharmacy and neurology at the University of Wisconsin-Madison who co-authored the study and worked as a consultant for the Epidiolex manufacturer. “There needs to be oversight so that patients know what they are getting.”
Some states, such as Michigan, have cannabis regulatory agencies. As such, Dr. Gregory Barkley, a neurologist at Henry Ford Hospital in Detroit, thinks that when a person shops at one of the state’s dispensaries, “you have a pretty good idea of what you’re getting.” Barkley regularly reviews his patients’ CBD products and discusses how many milligrams they take to help control their epilepsy.
But Barkley said CBD has inherent variability because it comes from a plant.
“It’s no different than saying, ‘I’m going to treat you with a Honeycrisp apple for an ailment.’ Every apple is a little bit different,” said Barkley. “The lack of standardization makes it difficult.”
About five years ago, Trina Ferringo of Turnersville, New Jersey, asked a pediatric neurologist about giving CBD to her teenage son, Luke, because his prescription drugs were causing severe side effects yet not preventing his epileptic seizures. The doctor was “adamantly opposed to it” because of the lack of FDA oversight and concerns it might contain THC, the chemical in marijuana that produces a high, Ferringo recalled.
Instead, in 2018, the doctor prescribed Epidiolex. Luke went from having several seizures each week to a couple per month. Ferringo is pleased with the outcome but now often fights with her insurance company because Epidiolex, which has a list price of $32,500 per year, isn’t approved for her son’s form of epilepsy.
Charlotte’s Web typically costs between $100 and $400 each month, depending on how much someone takes. Unlike Epidiolex, insurance never covers it.
Beyond the cost difference, it’s unclear whether a highly purified CBD product such as Epidiolex is more effective than products like Charlotte’s Web that contain CBD and other plant compounds, creating what scientists describe as a beneficial “entourage effect.”
A 2017 review of CBD studies in the journal Frontiers in Neurology, authored by scientists in the cannabis industry, found 71% of patients with treatment-resistant epilepsy reported a reduction in seizures after taking the CBD-rich products, but among patients taking purified CBD, the share was only 46%.
Patients taking CBD-rich products rather than purified CBD also reported taking lower daily doses and experiencing fewer side effects.
“Every cannabinoid when individually tested has a degree of anticonvulsant properties so that if you give a blend of various cannabinoids, they will have some additive effect,” Barkley said.
Changing CBD Regulations
Bipartisan legislation pending in Congress would designate CBD as a dietary supplement or food. The Senate version would allow the federal government to “take additional enforcement actions” against such products.
Jonathan Miller, general counsel to the U.S. Hemp Roundtable, a coalition of hemp companies, said the legislation would protect consumers and allow CBD manufacturers to sell their products in stores as dietary supplements.
However, Jensen Jose, counsel for the Center for Science in the Public Interest, said such legislation would actually make consumers less safe. The FDA does not have the authority to review dietary supplements for safety and effectiveness before they are marketed and does not routinely analyze their ingredients.
“If a CBD company right now is doing something questionable or potentially unsafe, the FDA can easily remove the product simply for being illegally marketed as a drug,” said Jose. If the legislation passes, he said, the FDA could not do that.
Instead, Jose said, Congress should provide the FDA with more authority to regulate CBD and dietary supplements and more funding to hire inspectors.
The FDA does not comment on pending legislation, spokesperson Courtney Rhodes said.
Patients like Taylor, the Colorado woman with epilepsy, aren’t waiting for the federal government. After the doctor’s visit, she borrowed money from family members and purchased a bottle of Charlotte’s Web.
“The effects were night and day,” she said. “I was able to get out of bed.”
She befriended a grower and spends about $50 per month on CBD powder, gummies, and oil. She now takes only one prescription medication for seizures rather than four. She has about one seizure per month, which means she can’t drive. Her medical providers still don’t seem open to discussing CBD, she said, but that doesn’t bother her much.
“After being on it for this many years and seeing the evidence — the 180-degree turnaround that my life made — it’s a choice I’m going to make whether they are with it or they are against it,” she said. “It’s working for me.”
Kaiser Health News is a national newsroom that produces in-depth journalism about health issues.