Wear, Tear & Care: The Quell Pain Relief Device
/By Jennifer Kain Kilgore, Columnist
When presented with the Quell pain relief device, people make one of two assumptions about me: 1.) I injured my knee, or 2.) I am a paroled felon wearing a very forgiving Velcro GPS.
As I said in my recent guest column, I have made it my mission to test as many pain relief products and therapies as possible. Some of them might be familiar to you; others will be of the “new and bizarre” variety. Whatever they are, I will be your Friendly Neighborhood Guinea Pig and review them for your convenience. I only draw the line at “Made for TV” products that are out to swindle the desperate consumer.
Pain patients are certainly desperate. We have a constant refrain humming through our bodies that plays a different tune for each person. Doctors are the musicians taught to hear those tunes -- but how can they possibly learn all the music? How can they hear your specific song and have the knowledge necessary to fix it?
The problem is that sometimes they cannot. They are deaf to your pain, just like that one whale who sings higher than every other whale -- none of them can hear her.
Thus far, doctors have been unable to hear the song that thrills along my nerve endings. This leaves me with no choice but to fend for myself. I could take the route at which they have hinted: find some street drugs and wait for the undertow to take me (not that this is the problem the media makes it out to be). Or I could travel a different road and at the same time realize that this life of mine includes pain. If I can’t get rid of it, I can at least muffle it.
image courtesy of neurometrix
As I said recently in my blog -- Wear, Tear, & Care -- I have been trying the Quell pain relief device, which is made in the great state of Massachusetts (i.e., my backyard). I have been using it every day for more than a month. Here are my findings:
- It absolutely works. I have been wearing it for 35 days. I assume there was some psychosomatic effect at first because I was so excited to try the device after months of hype. Once the initial thrill wore off, I was left with the knowledge that, yes, I have reduced my number of Motrin from 16 a day to four, give or take. I am still on Cymbalta and Lyrica for pain control and situational depression, though I can now contemplate reducing the Lyrica entirely. Before, that was not even a possibility.
- Wearing any kind of medical device during the summer is difficult. I can make the Stride of Pride and show if off with a skirt or shorts; otherwise I have to find pants under which the device can comfortably fit. This means that a good portion of my wardrobe (leggings, skinny jeans, etc.) is not compatible with the Quell. This is a minor concern.
- The Quell is $249.00. Replacement electrodes cost $30 and last for two weeks. I have worn mine for longer than that because A.) I can, and B.) I’m cheap. The electrodes break down quickly, but as a whole they are more durable than traditional electrodes and do not irritate my skin. With the EMPI device, the electrodes left blisters on my back.
- The iPhone app is quite lovely. It has a countdown clock so you can see how long the therapy has lasted or how far away it is. I have become adept at the internal calculation of 60 minutes on, 60 minutes off.
- Unlike other TENS devices I have tried, the stimulation is not distracting, so wearing it at the office is fine.
This is all well and good. But how does the Quell work?
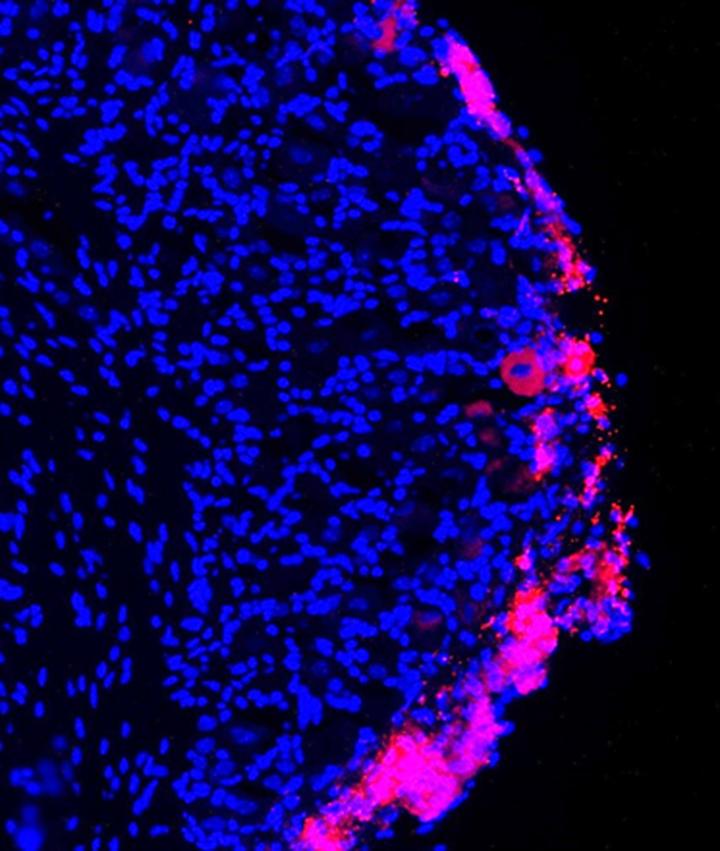
According to their research paper presented to the FDA, the Quell works not unlike other devices that latch onto a dense cluster of nerves in the upper calf. Generally it is best for lower-body pain (sciatica and the like), diabetic neuropathy, and fibromyalgia. I myself have fibromyalgia-ish symptoms, since my pain radiates all over my body. However, I apparently do not actually have the inflammation that is fibro’s hallmark. Doctors will only commit to “chronic pain syndrome.” Since the device works for me, I can say confidently that it treats more than those three conditions.
The Quell is twice as strong as conventional TENS units, does not irritate the skin like traditional electrodes, is less conspicuous, has a mobile app, and can be worn at night. (They say it can be worn at night; I personally found the stimulation too distracting.) It activates endogenous opioids in the body (natural opioids, to say it in English), a different system than the one on which prescription opiates work.
It is, simply put, a wearable intensive nerve stimulator that follows the Pain Gate Theory: The impulses generated by the Quell block pain signals from reaching the brain. As it was cleared to be sold over-the-counter, it is currently not covered by insurance.
I know you pain patients out there loathe the numbers system (What is your pain on a scale of 1 to 10?). I also despise it; this is the only one that has come close to working for me. That’s why I have created a new system. Instead of assigning an arbitrary number to my pain, I am going to tell you what I can do now that I couldn’t do before.
1. I can cut down my daily over-the-counter medication.
2. I can walk for longer periods of time (36 days ago I could walk about 10 minutes before starting to limp; now I can make it almost 30 minutes).
3. I can sit for longer periods of time during the work day (prior to the Quell I’d last 10 minutes before having to get up and move around; now I can make it to 30 before movement becomes necessary).
4. I can focus better on immediate tasks.
5. I have more energy during the daytime, which makes me more social. I have been hanging out with friends more. However, I still practice the chronic pain version of sundowning in the evenings (i.e., I crash).
6. I have been able to resume my almost-daily yoga practice. I even did a 55-minute video the other day (which was Aroga Yoga’s yoga class for those with chronic illness).
7. I have been able to resume my aqua aerobics practice two to three times per week.
8. I wear my emergency back brace less frequently.
9. I have fewer flares.
FINAL DIAGNOSIS: The Quell device has worked brilliantly for me. While it doesn’t get rid of all the pain I feel, it dampens enough of it so that I can more fully live my life. I hope that it can bring others as much relief.
Jennifer Kain Kilgore is an attorney in the Greater Boston area who also works as a writer and editor in her spare time. She has chronic back and neck pain after two car accidents.
You can read more about J.W. on her blog, Wear, Tear, & Care.
The information in this column should not be considered as professional medical advice, diagnosis or treatment. It is for informational purposes only and represents the author’s opinions alone. It does not inherently express or reflect the views, opinions and/or positions of Pain News Network.